PUBLIC hospital ramping is at record levels. Public hospital waiting lists are unmanageable. Yet, public hospitals across Australia are admitting massive and disproportionate numbers of private patients. It's a perverse reality.
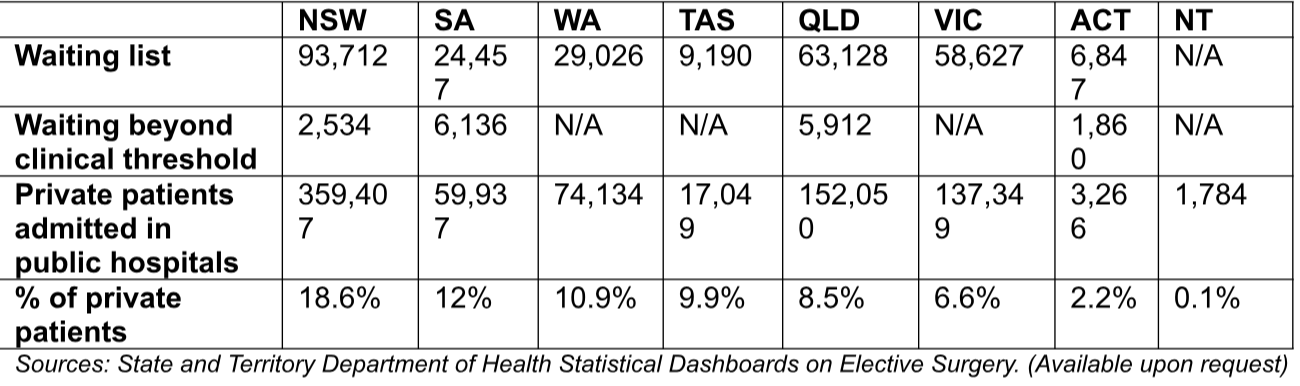
According to data from each state government, there are 284,987 public patients languishing on public hospital waiting lists across the country. More than 16,000 patients, that we know of, are waiting beyond the clinical threshold for the treatments they need. That means their condition deteriorates, they develop co-morbidities, and their mental health often suffers the longer they wait.
But over the last year public hospitals admitted 804,976 private patients. A decade ago, only 7% of patients treated in public hospitals were classified as private. Today, that figure has climbed to 11% nationally. The latest state-by-state numbers paint a stark reality.
The Australian Private Hospitals Association and Catholic Health Australia are united in calling on the Federal Government to strengthen its hand in the current National Health Reform Agreement negotiations.
Public hospitals and state governments should no longer receive federal funding for private-in- public activity. If state-run public hospitals admit private patients, they should shoulder the gap between what Medicare and insurers pay, instead of passing it onto the taxpayer.
The last five-year agreement saw taxpayers pay some $400 billion for public hospitals and their patient loads. The next agreement should come with the caveat that public patients, especially those that cross the line for their clinical wellbeing, should immediately be transferred and treated in a private hospital at the state's expense.
Quotes for attribution:
Brett Heffernan, CEO, Australian Private Hospitals Association:
"If state governments prioritised public patients, waiting lists might soon not exist and ramping could be a thing of the past as more beds are freed up from those jumping the queue.
"It's no secret that state governments are addicted to the revenue they receive from privately insured patients, but when so many public patients are pushed to the back of the queue and are waiting longer than necessary for their surgery, it becomes very hard to justify.
"These measures may motivate state governments to pay more than lip-service to public hospital waiting lists. It's not unreasonable for the Federal Government to insist that public patients no longer be second-class citizens and hold states who continue to rack up disproportionate private patient caseloads to account."
Dr Katharine Bassett, Director of Health Policy at Catholic Health Australia:
"Public hospitals were founded on the principle of need, not entitlement. They are meant to help people who need them most - not those who have the money and status to jump the queue.
"The more this happens, the more the balance of our health system breaks down. Public patients wait longer while private hospitals struggle to remain viable.
"The incentives drawing private patients into public wards must be wound back. Public hospitals and state governments should no longer receive Commonwealth funding under the National Health Reform Agreement for private-in-public activity.
"That way, if public hospitals and States decide to admit private patients, they could no longer claim and pocket extra funding on top of what Medicare and insurers pay."