A new immunosensor based on Quenchbody technology shows great potential as a fast, inexpensive, and convenient tool to detect SARS-CoV-2. Developed by scientists at Tokyo Institute of Technology (Tokyo Tech) and Tokyo Medical and Dental University (TMDU), this highly efficient diagnostic approach will be useful not only for point-of-care testing, but also for high-throughput epidemiological studies of COVID-19 and other emerging infectious diseases.
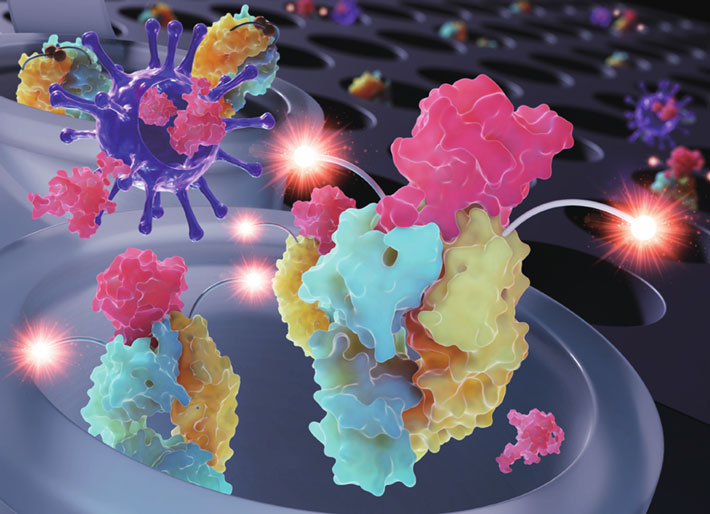
Figure 1. Detecting SARS-CoV-2 with a new Quenchbody immunosensor
The double-tagged Quenchbody immunosensor becomes fluorescent when its target antigen—the nucleocapsid protein from SARS-CoV-2—binds at the antigen-binding region of the antibody fragments. This approach is fast, cost-effective, and convenient to use in practice, making it ideal for point-of-care testing as well as batch processing of patient samples. The above image, which illustrates how the immunosensor becomes fluorescent upon antigen binding, was selected as the back cover for Issue 22 of the Analyst journal.
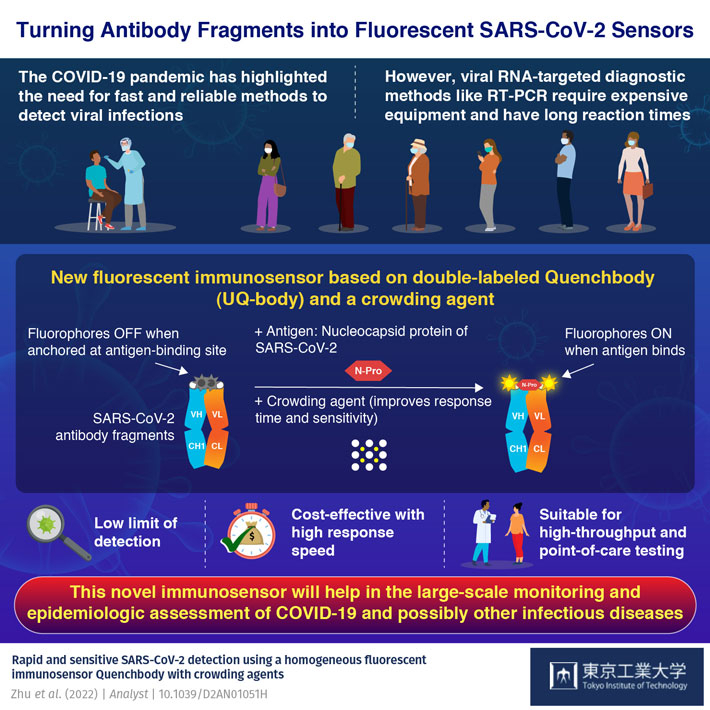
The incredibly fast spread of COVID-19 throughout the world brought to light a very important fact: we need better methods to diagnose infectious diseases quickly and efficiently. During the early months of the pandemic, polymerase chain reaction (PCR) tests were one of the most widely used techniques to detect COVID-19. However, these viral RNA-based techniques require expensive equipment and reaction times longer than an hour, which renders them less than ideal for point-of-care testing.
The limitations of PCR fueled the development of various immunoassay methods, which use specially engineered antibodies to detect SARS-CoV-2 antigens with high sensitivity in little time. Today, scientists are still improving immunoassay technology to make available tools more convenient, sensitive, and cost-effective.
Against this backdrop, a team of researchers led by Professor Hiroshi Ueda from Tokyo Institute of Technology (Tokyo Tech), Japan, has been working on a promising emerging technology for diagnosing COVID-19 and possibly other infectious diseases. Their latest paper, which was published in Analyst, not only details a new Quenchbody fluorescent immunosensor that can detect SARS-CoV-2 with exceptional speed and sensitivity, but also a simple way to greatly enhance the immunosensor's performance using a crowding agent.
But what exactly are Quenchbodies? A Quenchbody is a molecular sensor originally developed by Professor Ueda and colleagues using antibody fragments and fluorescent tags. The antibody fragment, which can be an antigen-binding region (or 'Fab'), targets a specific viral molecule (antigen). Meanwhile, the fluorescent tags are small fluorescent dye molecules attached by a peptide linker to the Quenchbody, near the antigen-binding region. When the antigen is absent, the fluorescent tags are attracted to the Fab and intrinsic amino acids (mainly tryptophan) interact with the dyes and quench the fluorescence. However, when the antigen appears, it replaces the fluorescent tag at the Fab, causing it to move away and recover its fluorescence. Thus, in a Quenchbody test, an increase in fluorescence indicates the detection of the target antigen (as shown in Figure 1).
In this study, the research team developed a double-tagged Quenchbody targeting the nucleocapsid protein (N protein) of SARS-CoV-2. To take things one step further, they also tested whether various commercially available compounds could improve the immunosensor's sensitivity and detection time. In particular, adding polyethylene glycol 6000 (PEG6000) at the right concentration as a crowding agent increased performance quite significantly. "The enhanced limit of detection against the N protein was lower than 0.3 nM within 5 minutes of incubation, which is an order of magnitude more sensitive than without adding a crowding agent," remarks Professor Ueda.
To further validate their approach, the team tested their immunosensor on leftover clinical samples from COVID-19 positive patients. After careful analysis of the results, they concluded that their newly developed Quenchbody could measure N protein more easily and quantitatively than a commercial lateral flow antigen test. Excited about these findings, Professor Ueda concludes: "Our work shows the feasibility of using Quenchbody immunosensors as rapid and cost-efficient tools for the diagnosis and high-throughput analysis of swab samples in large-scale monitoring and epidemiological studies of COVID-19, as well as other emerging infectious diseases."
This study was selected to be included in the Analyst HOT Articles 2022 collection and also featured in the back cover of Issue 22 of the journal (shown in Fig. 1). Let us hope this helps bring Quenchbody technology to the limelight so that we can be better prepared to deal with future pandemics.
Reference
Authors : |
Bo Zhu1#, Nobuyuki Nosaka2#, Shuji Kanamaru3, Jinhua Dong1,4,5, Yancen Dai3, Akihito Inoue3, Yinghui Yang3, Kaori Kobayashi3, Tetsuya Kitaguchi1, Hiroshi Iwasaki3,6, Ryuji Koike7, Kenji Wakabayashi2 and Hiroshi Ueda1,5*
# Contributed equally |
Title : |
Rapid and sensitive SARS-CoV-2 detection using a homogeneous fluorescent immunosensor Quenchbody with crowding agents |
Journal : |
Analyst |
DOI : |
|
Affiliations : |
1 Laboratory for Chemistry and Life Science, Institute of Innovative Research, Tokyo Institute of Technology 2 Department of Intensive Care Medicine, Graduate School of Medical and Dental Sciences, Tokyo Medical and Dental University 3 Graduate School of Life Science and Technology, Tokyo Institute of Technology 4 School of Rehabilitation Science and Engineering, University of Health and Rehabilitation Sciences 5 World Research Hub Initiative (WRHI), Institute of Innovative Research, Tokyo Institute of Technology 6 Cell Biology Center, Institute of Innovative Research, Tokyo Institute of Technology 7 Medical Innovation Promotion Center, Tokyo Medical and Dental University |






