
When it comes to personal medical care, most Americans say they're satisfied. Nearly eight in 10 rate their own doctors and clinics as "very good or excellent." Yet that same public voice reveals deep unease with the system around them. Nearly nine in 10 say the U.S. health system is either staying the same or getting worse, and eight in 10 believe it needs major reform or a complete rebuild.
Those findings anchor the People's Voice Survey, a global effort to understand how people experience, trust and value their health systems. The survey's first publicly released U.S. results were unveiled Oct. 29 by the Washington University in St. Louis QuEST Center, in partnership with the School of Public Health, during the Science for Health Systems inaugural conference, held at WashU and online.
The 2025 data, drawn from 4,066 adults nationwide, form the basis of a new "People's Report Card" grading the nation's health system on access, affordability, quality and trust.
"We want to know: Is the health system working for people? How do people rate it? And how have perceptions changed?" said Todd P. Lewis, PhD, People's Voice lead researcher and an assistant professor in the Division of General Medicine and Geriatrics at WashU Medicine, who presented the findings.
How the survey works
Margaret E. Kruk, MD, is director of the universitywide QuEST Center and the international QuEST Centers and Network, and the Distinguished Endowed Professor of Health Systems & Medicine. Her leadership on the The Lancet Global Health Commission on High-Quality Health Systems in 2018 laid the groundwork for the People's Voice Survey - now implemented in 22 countries. The commission established that health systems exist first and foremost for people, and must be judged not only by outcomes but by trust, competence and experience.
The U.S. survey was first conducted in 2023 as a nationally representative study and expanded with a larger sample in 2025. Respondents were recruited from a representative panel of adults, balanced by age, gender, race and ethnicity, and region. An additional oversample in Missouri - home to WashU and its new School of Public Health - enabled detailed state-level analysis of local experiences. This collaboration with the School of Public Health expanded the overall sample size and allowed a focused look at Missouri.
The survey used telephone or online sampling to measure how people access care, what barriers they face and how confident they feel in the system's ability to meet their needs.
A nation of high users
Americans are among the world's heaviest health-care users, averaging seven contacts per year - six in-person visits and one telehealth appointment. Nearly half said their most recent visit was for prevention or a routine checkup. Preventive screenings remain consistent with U.S. guidelines - for example, 84% of Americans reported having a blood pressure check within the past year.
Telehealth has remained steady since the pandemic. The United States ranks second only to the United Kingdom in telehealth use, and 72% of users rated their virtual care "very good or excellent" - the highest satisfaction of any country surveyed.
But public opinion shifts when people think beyond their own doctor's office. When asked to rate community-level services, such as care for women, children and people with chronic diseases, only about six in 10 Americans gave high marks. Just four in 10 rated mental health care in their communities positively. The data suggest that while the health system often works for individuals, confidence erodes when people look at how it serves their neighbors.
Faltering trust
The 2025 survey shows that two-thirds of Americans (63%) feel confident they could both get and afford care if sick tomorrow - a five-point improvement since 2023 and the third-highest rate among high-income countries.
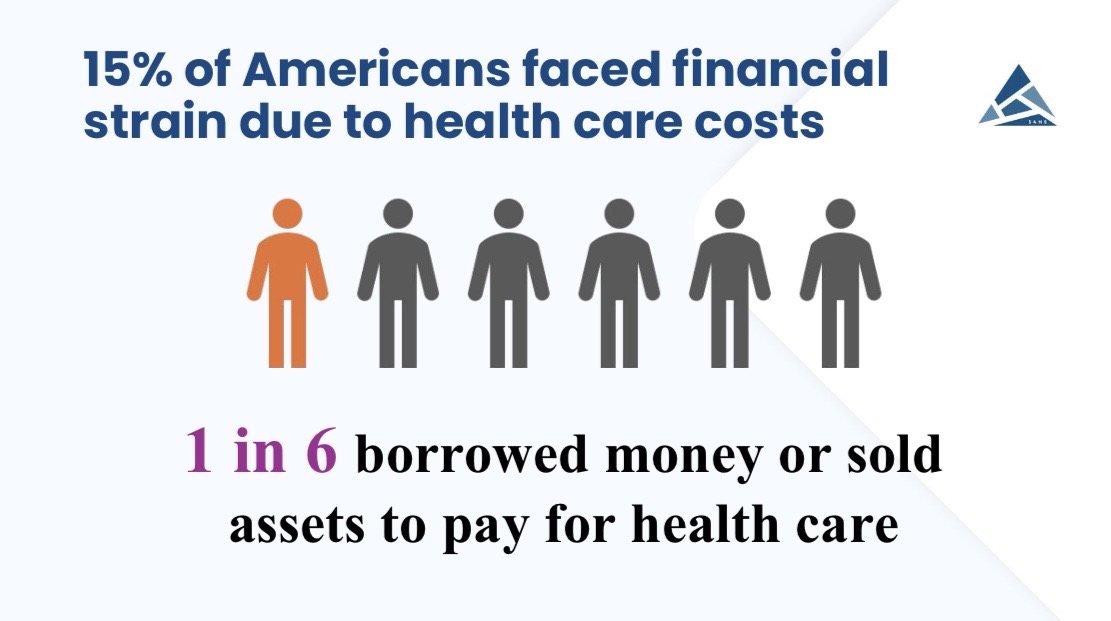
Yet beneath that confidence is a steady undercurrent of strain and skepticism. One in six Americans reported borrowing money or selling possessions such as furniture or jewelry to pay for care. Another 15% went without needed care entirely, most often due to cost or poor patient experience. Both numbers have risen since 2023.
Despite feeling more secure personally, 88% believe the system as a whole is either stagnant or declining, in need of major reform. Only one in three Americans believe government leaders consider public opinion in health decisions, and just one in five say the U.S. handled the COVID-19 pandemic well.
The paradox of personal satisfaction versus systemic frustration dominated a panel discussion following the report's presentation at the conference.
"Eighty percent of the people love their own personal health care, love their doctor, but they hate the damn system," said panelist Timothy D. McBride, PhD, the Bernard Becker Professor at the WashU School of Public Health and co-director of the Center for Advancing Health Services, Policy & Economics Research. "And about 18 to 20% of people they know struggle to get access or pay for care. That may explain how you can be personally happy but still think the system's broken."
He added that the divide mirrors broader inequality. "The economy seems to be doing well, but not for everyone. It's the same with health care. It's working for most of us on this stage, but not for the 15 to 20% being left behind."
Sandro Galea, MD, DrPH, also on the panel, agreed, pointing to the societal implications. "The poorest 40% of Americans are much more vulnerable than everybody else," said Galea, the Margaret C. Ryan Dean of the School of Public Health and the Eugene S. and Constance Kahn Distinguished Professor in Public Health. "These are, unfortunately, the same people who are currently most affected by the government shutdown. We have as a country been far too willing to leave people behind, and those of us whose responsibility it is to promote health need to be persistent in making a moral and practical case for not doing so."
A closer look at Missouri
Because Missouri was oversampled, researchers were able to identify state-level trends.
Compared with the national average, Missourians reported poorer overall health and mental health and higher rates of chronic illness, indicating a generally sicker population. Yet they also showed greater engagement in their health - both in managing care and in feeling confident sharing concerns with their doctors.
Ninety percent of Missourians said they have a usual source of care, compared with 83% nationally. Preventive care rates and quality ratings for personal visits were similar to national averages.
The state's largest deficits appeared in unmet need and financial strain. Seventeen percent reported going without needed care v. 15% nationally, and one in five (20%) said they borrowed money or sold assets to pay for care. Only 57% felt confident they could both get and afford care if needed.
"Missouri does not do well on a wide variety of social determinants of health," said panelist Spring Schmidt, CEO and president of the Missouri Public Health Institute and director of public health practice at Saint Louis University College for Public Health and Social Justice. "We can't take the system out of the social context that it's actually operating in."
Mental health gaps
Mental health care stood out as one of the lowest-rated areas in the national People's Voice Survey - earning an F grade on the report card and lower confidence than any other service area.
Eighteen percent of Americans screened positive for possible depression, using a supplementary personal health questionnaire.
The most common treatment pattern combined professional care and self-care, reported by 47% of respondents. Another 17% relied solely on self care, while 30% received no support. Most began with a primary-care doctor, followed by psychiatrists or psychologists.
Self-care was common: 28% exercised, while others practiced mindfulness or meditation or used digital tools such as apps, online forums and informational websites.
Grading the system
To summarize findings, researchers issued a People's Report Card, benchmarking the United States against six other high-income nations.
Grades were assigned using a conservative scale - A (80% and above), B (70-79), C (60-69) - to enable cross-country comparison.
- Preventive care: C grade overall, second behind Italy
- Barriers to care: Most Americans avoided unmet need or financial strain (A grades when measured alone), yet the United States ranked near the bottom globally - meaning other high-income countries reported fewer barriers to care.
- Quality of care: B grades for both telehealth and in-person visits - first among peers
- Community care: two C's for women's and children's care, a D for chronic disease management and an F for mental health
- Insurance coverage: A for private insurance, B for Medicaid
- Confidence indicators: C for health security, D for the system's direction
- Leadership: failing grades for pandemic management and public voice inclusion
An interactive dashboard, built by the Digital Intelligence and Innovation Accelerator (led by Dan Maranan, executive director, with WashU students Julie Baguio, John Li and Justin Park, and supported by Betsy Sinclair and Nathan Jacobs, assistant vice provosts for digital transformation, and Executive Vice Provost Mary M. McKay) allows users to explore results by region and demographic group.
Global health and impact
For Kruk, who has led international efforts to measure health-system quality, the People's Voice Survey closes a critical gap.
"What we deeply want is policy impact," she said. "We want systems to change on the basis of this data."
The results are already informing policy dialogues in Peru, strategic planning in Ethiopia and national debates in Nigeria. As panelist Chike Nwangu observed, "If people don't believe in the quality of service they're receiving, they won't come back." Nwangwu is CEO of NOIPolls Limited in Nigeria. "You can do all your strengthening, but if you don't build belief, you won't have a system."
McBride added that engaging citizens directly is essential to that charge. "The citizens' voice is important," he said. "Let's be honest about who's talking to policymakers - it's the providers, the systems leaders, the business leaders. The citizens are not always in the room."
Galea broadened the conversation: "Health is one of the truly universal human values," he said. "All people want to live longer, healthier lives - and yet no country has fully figured out how to build a system that meets that need. Systems once held up as models, such as Canada and the U.K., are now facing high levels of dissatisfaction. That tells us the turmoil is real and shared.
"It's enormously complex to build health systems that are high quality, affordable and reach everyone," he added. "That's why we need science and evidence to guide us - and then we need to do the really hard work."
As the People's Voice expands, WashU's leadership is at the forefront of understanding not just how systems function, but how people feel about them.
Kruk closed the session with a simple reminder: "Health systems exist for people."






