A team of researchers at Cornell University have made a discovery in fruit flies that could change the way we understand brain diseases like Alzheimer's and Parkinson's in humans.
The scientists found that Eato-a fruit-fly protein whose counterparts in mammals were already known for helping brain cells get rid of harmful fats-actually has a much bigger job. It not only protects neurons (brain cells), from being destroyed, but also increases the efficiency by which other cells, called phagocytes, clean up damaged neurons. The researchers used Drosophila fruit flies, which are commonly used in experiments because they have many of the same basic biological processes as humans.
Bei Wang, Chun Han and Nicolas Ruiz in the laboratory at the Weill Institute for Cell and Molecular Biology.
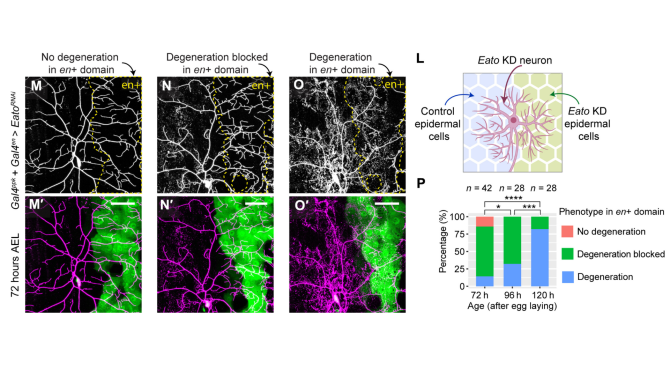
Xinchen Chen, a doctoral student working with Chun Han, a Nancy M. and Samuel C. Fleming associate professor in Molecular Biology and Genetics at the College of Agriculture and Life Sciences and Cornell's Weill Institute for Cell and Molecular Biology, discovered that when Eato was missing from neurons, those neurons died, but not on their own. Instead, phagocytes were employed to kill and eat the neurons.
The study, which could suggest new treatment strategies for neurodegenerative disease like Alzheimer's, was made possible by a grant from the National Institutes of Health, and a Multi Investigator Seed Grant from Cornell University. It published in Science Advances in March.
The researchers found that when brain cells are stressed or starting to die, a special "eat-me" signal appears on their surface in the form of a fatty molecule called phosphatidylserine (PS) that flips to the outside of the cell. This PS signal acts like a flag telling phagocytes, "this neuron can be cleaned up and engulfed," and helps the phagocytes avoid mis-identifying the target of destruction.
Normally, Eato helps keep that flag hidden when cells are still healthy. But without Eato, PS shows up too early-even if the neuron isn't really damaged-causing phagocytes to destroy perfectly good brain cells. This points to potential therapeutic pathways to stop neurodegeneration in diseases like Alzheimer's and Parkinson's.
Eato is a member of the protein family called ABCA transporters, which consists of membrane proteins crucial for maintaining proper lipid homeostasis in cells. It is already known that two human ABCA transporters (ABCA1 and ABCA7) are associated with Alzheimer's Disease, said Han. A few more are related to other kinds of neurodegenerative diseases.
Alzheimer's disease is the most common cause of dementia and the fifth leading cause of death in adults older than 65 years, becoming more common as the population ages. In 2020, Alzheimer's care cost about $305 billion, and that number could pass $1 trillion in the future.
A study by the Michael J. Fox Foundation found the total cost of Parkinson's disease to individuals, families and the United States government is $51.9 billion every year, with $25.4 billion attributable to direct medical costs (e.g., hospitalizations, medication) and $26.5 billion in non-medical costs like missed work, lost wages, early forced retirement and family caregiver time.
"We have been working on how phagocytes eat neurons since 2018 when we established a system to see PS exposure on neurons in Drosophila," Han said. "Since then, we have been studying how PS is regulated in neurons and how PS exposed on the surface of neurons is recognized by phagocytes… ABCA lipid transporters are good candidates for regulating PS exposure, so we checked them and found Eato."
The discoveries, however, were not what was expected. The team found that if Eato is removed from both neurons and phagocytes, the damage declines, showing that Eato has a double role-it both protects neurons and helps phagocytes detect PS exposed on neurons.
"Eato's dual role in suppressing phosphatidylserine (PS) exposure is completely surprising and was not predicted based on previous findings on other ABCA transporters," Han said. "Eato seems to work differently in neurons and glia, even though in both cell types it suppresses PS exposure."
Han and his team believe these findings could eventually lead to new ways to treat diseases like Alzheimer's by stopping healthy neurons from being mistakenly removed. In fact, they even found that removing PS exposed on Eato-deficient neurons prevents neuronal degeneration.
"The mechanisms we discovered for Eato are very novel, and they suggest pathways that could contribute to these neurodegenerative diseases," Han said. "The current work focuses on fundamental mechanisms…but I can imagine treatments that target either surface PS exposure or glia's ability to see PS exposure on neurons may be useful for preventing the progress of the neurodegenerative diseases."
By understanding how proteins like Eato work, the Weill Institute scientists hope to find ways to slow down or even prevent some of modern medicine's most stubborn and malicious diseases. For now, this research is a step closer to unlocking some of the brain's biggest mysteries.
Other contributors included Bei Wang, Ankita Sarkar, Zixian Huang, Nicolas Vergara Ruiz, Ann T. Yeung, and Rachael Chen, all from the Weill Institute for Cell and Molecular Biology at Cornell University.
Henry Smith is the communications specialist for biological systems at Cornell Research & Innovation.