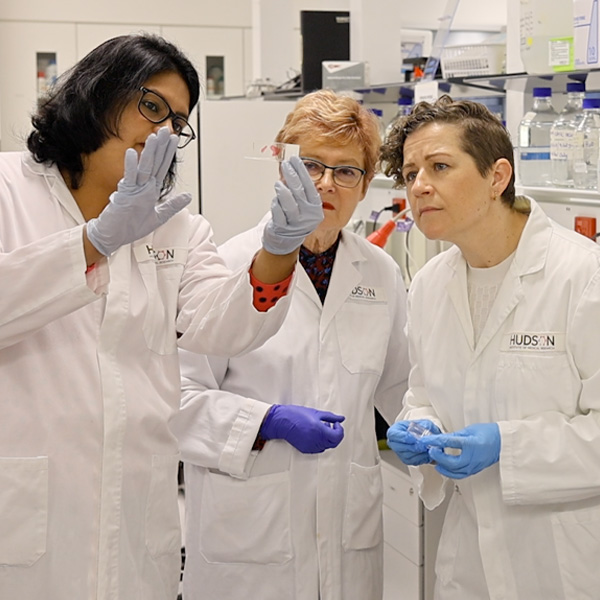
Two women from different backgrounds met for the first time at Hudson Institute because they have one thing in common. For Associate Professor Shayanti Mukherjee, born in India and now living and raising her family in Melbourne, it's her life's work; For Sally Maconochie, Brisbane major projects consultant and mother, it is the thing that turned her from a super-fit marathon runner to a person living with a disability.
The 'thing" in question is pelvic organ prolapse (POP), a common medical condition, that many have never heard of. POP develops when tissues, pelvic floor muscles and ligaments that support the pelvic organs (bladder, uterus and bowel) become damaged, usually in childbirth, causing organs to shift or 'drop' into or outside the vagina. POP is essentially a hernia through which organs protrude because supporting tissue is weak.
Horrifying and traumatic
In Sally's words, the impact on her life was horrifying and traumatic, so severe that she decided to find out as much as she could about POP and spread the word. That is how she found Hudson Institute.
"The way the prolapse affected me in everyday life was quite obvious and something I found I couldn't hide - I couldn't stand for 10 minutes, let alone run." – Sally Maconochie
A/Prof Mukherjee, Head of the Translational Tissue Engineering Research group, specialises in innovative cell-based therapies for pelvic floor disorders and birth trauma injuries.
Next-generation therapies
She and her team are designing degradable meshes to regenerate vaginal tissue using a polymer material approved by the US Food and Drug Administration (FDA), to create tissue engineering therapies for treating POP. It is a vexed area of research since the surgical use of synthetic, non-degradable meshes was banned after they were found to be responsible for serious and life changing damage in a significant number of patients.
Her team combines engineering and 3D printing expertise with Hudson Institute's own stem cell technologies to develop a safer alternative that works with a woman's body, not against it.
It is no wonder that when they met in the lab, Sally and Shayanti had plenty to discuss. "The 3D bio-printed mesh is something I'm really excited about," Sally said. "The fact that Hudson Institute is looking at a potential mesh alternative is really exciting, because for people like me who have muscle away from bone, that's the only way we have of re-attaching it."
Prevention and cure
Hudson Institute's team are focused on prevention, as well as a cure. Building on Professor Caroline Gargett's research with mesenchymal stem cells, A/Prof Mukherjee is also working to develop ways to better identify and treat birth injuries when they happen, rather than waiting until they develop into something much more serious, like POP, in later years.
Sally wants to do whatever she can to ensure that future generations of women are better prepared and informed as they approach birth. "My mother, my grandmother and her other all had prolapses after childbirth, but no-one mentioned it to me until it was too late, and it turns out that a family history of prolapse is one of the biggest risk factors."
The researcher and the advocate now have a mutually beneficial relationship, born of pain but promising so much joy and relief for women everywhere.