CU Anschutz providers bring research into specialized clinic care to advance diagnosis and treatment for military members and beyond
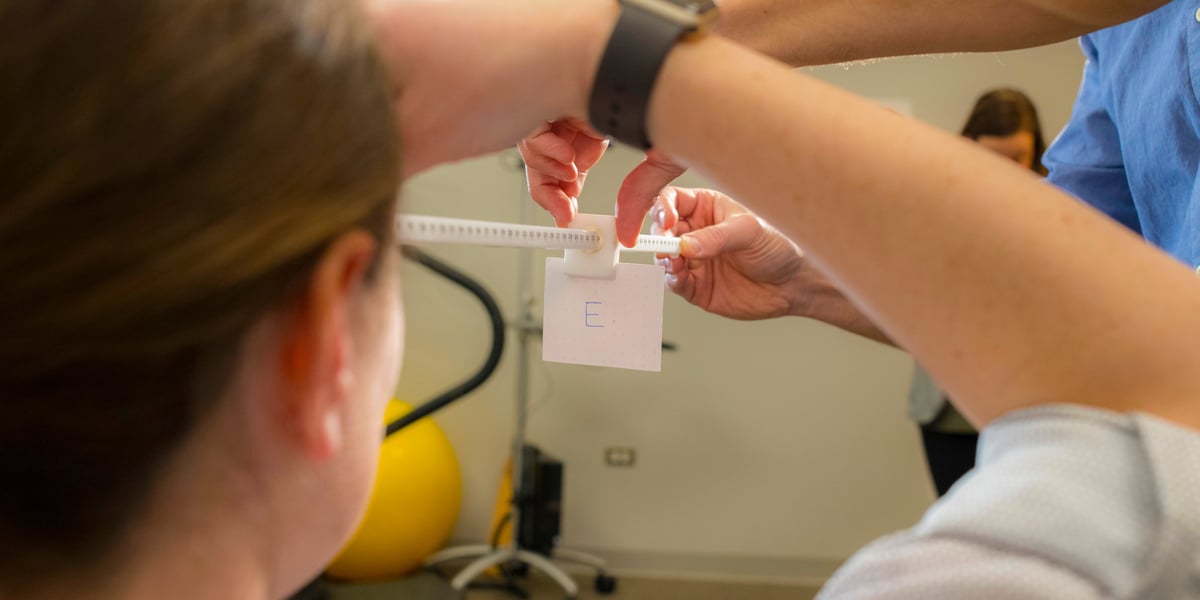
When Jeffrey Hebert, PhD, peers into a patient's eyes, he can't always see what he wants to see.
As a physical medicine and rehabilitation specialist at the Marcus Institute for Brain Health (MIBH), Hebert examines many people with vision-trouble complaints that are often vague yet life-altering.
"Often, we'll do a vision exam, and their visual acuity is good. They are 20/20 on the eye chart exam. Their vision tracking looks clean. But they'll still say: I don't see things well. I can't retain what I read. I just don't take things in."
That's when Hebert takes a deeper look.
Many of his patients are military members and veterans with prior mild to moderate traumatic brain injuries (TBIs). Because the body's senses are central to brain function and cognition, vision troubles can be an indicator of TBI.
"As humans, we take in information from the outside through our senses, and the brain immediately begins processing and coding it; it's called bottom-up processing," Hebert said. "In an injured brain, especially one with repeated mild TBI, or concussions, that first crucial processing step is often disrupted."
Hebert - who earned his PhD because he no longer wanted to "wait for evidence" for his patients; he wanted to be "part of creating the evidence" - is director of research at the MIBH.
Blocking a road to solitude
Visual function and processing breakdown - along with cognitive and emotional symptoms of TBI - can shorten military careers and make reintegration into non-military life overwhelming, Hebert said.
"The civilian world is a lot less structured, a lot more variable and even busier sometimes. You go into a busy restaurant, you go into the grocery store, and there's just a lot of stuff going on for any human. But for a veteran with prior brain trauma, it is much more difficult and dysregulating."
His patients, which also include first responders, can become overwhelmed, confused and frustrated by sensory overload. And, as emotional control is also commonly dysregulated, they might lash out, be irritable and feel angry all the time, he said.
"They will say: 'I don't know why I don't like the grocery store. I don't know why I don't like crowds and restaurants.' And a key element could be the difficulty of managing multisensory input in those environments."
The next common response is to retreat, avoiding those activities all together, Hebert said.
"They start to isolate themselves and take themselves away from interaction with other people, which can lead to further cognitive decline and emotional dysregulation. So, it's key for us as clinicians and researchers to provide the why - why is this happening - and continue investigating ways to help."
CU Anschutz is a national leader in military medicine, uniquely positioned within 45 minutes of seven military bases and home to top experts in the field. Advancing care for service members and translating that research into the civilian sector is a primary goal.






