Joseph spent his childhood dreading family gatherings. His Egyptian-American relatives would gather around the family table for traditional fare—pita, falafel, baba ghanoush—while Joseph sat by himself, eating food his parents had brought from home. With multiple food allergies, Joseph needed to maintain an exhausting level of vigilance to avoid potentially lethal allergens, and that often meant eating alone. Shared meals, normally a source of fellowship and connection, became moments of painful isolation.
Joseph's experience is unfortunately not unique: Food allergies affect around 15 million people in the United States, including 6 million children. People with allergies as severe as Joseph's, especially those allergic to multiple foods, have no options aside from avoiding trigger foods while carrying an epinephrine auto-injector in case of accidental ingestion.
But avoidance isn't so simple, since even miniscule exposures can lead to severe reactions and accidental ingestion can happen even to the most vigilant people. That regular routine of avoidance and fear of reactions can drastically alter the quality of life of both people with allergies and their families.
Kids who can't participate in classroom snack times or birthday parties often endure bullying. Parents might spend hours at the grocery store scanning food labels, searching for nutritious food that won't harm their child. And on top of that is the anxiety of uncertainty—accidental exposure might not cause life-threatening anaphylaxis, but it certainly can. The mental toll is enormous, says Kim Mudd, nurse manager of the food allergy research program at the Johns Hopkins Children's Center.
"If you ask parents, 20% of parents say they think that their child is at a moderate or severe risk of having a fatal anaphylactic event," she says, "yet they still have to send their kids off to school every day."
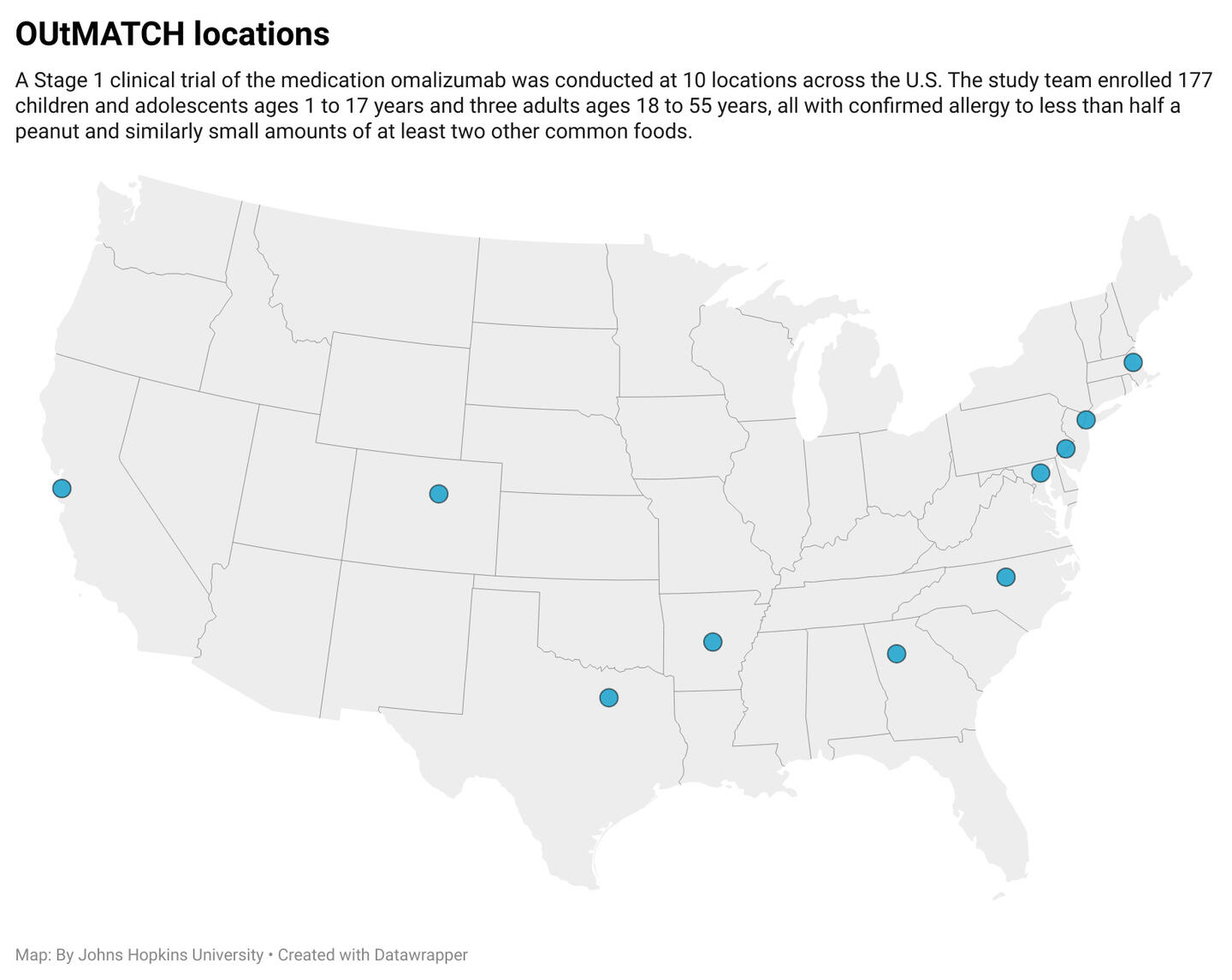
Given the magnitude of food allergy for so many, in 2005 the NIH established the Consortium for Food Allergy Research, or CoFAR, to support clinical research on food allergies. CoFAR began with five centers and now consists of 10 participating universities and hospitals across the country, ranging from Arkansas to California to North Carolina. Johns Hopkins acts as the Leadership Center under the direction of Robert Wood, director of the Eudowood Division of Allergy, Immunology, and Rheumatology at Johns Hopkins Children's Center and director of the Leadership Center since 2017.
Since its establishment in 2005, CoFAR has emerged as a world leader in establishing best practices in allergy treatment and management. It was recently awarded $77 million for seven more years of funding to support potential treatment or prevention trials and local food allergy-related clinical studies at individual CoFAR sites.
Part of the team's success stems from its size and geographical reach. A diverse patient pool allows researchers to better evaluate a drug's ability to work for multiple demographics, and having access to leading allergy experts across the country was also crucial to the study's success.
"It's team science," Wood explains. "Instead of having all 10 of us competing for whatever money the NIH is going to use for food allergy, we're doing that research as a group."
CoFAR's multistate alliance enabled Wood and his team to launch the groundbreaking OUtMATCH study in 2019. This clinical trial's results have changed the landscape of food allergy management by showing that the drug omalizumab, marketed as Xolair, reduces the severity of allergy symptoms for people who take it regularly, significantly lowering the chance of anaphylaxis or other severe symptoms after accidental ingestion. Originally approved to treat severe asthma in 2003, omalizumab was approved by the U.S. Food and Drug Administration in February 2024 to also include treatment of food allergies in patients over age 1 based on the results of the OUtMATCH study.
Xolair works by blocking the action of the IgE antibodies that cause allergic reactions, thereby treating any food allergies. This is only the second FDA-approved treatment for food allergy, with the other being a product that only treats peanut allergy. Indeed, this work is so groundbreaking that Wood was named among the Time100 Most Influential People in Health of 2025.
"About 50,000 people have begun using this drug in just a little over a year," Wood said. "That's one of the fastest uptakes of any drug ever. So it really speaks to the unmet need and how important this research is."
With 10 research sites across the country, OUtMATCH was able to screen 479 allergic participants and enroll 180 in the study, making it the biggest of its kind ever conducted. For 16 to 20 weeks, enrollees were randomized to receive either a placebo injection or omalizumab.
The project was able to move much more quickly than it would've had it been conducted at just one hospital.
"If we had had to screen 479 patients [at Johns Hopkins], we'd still be enrolling participants," Mudd says. "Having the ability to spread that out across 10 sites certainly makes the logistics much more feasible."
The study recruited participants with serious allergies to multiple foods. To be eligible for the study, participants had to demonstrate reactions during double-blind, placebo-controlled food challenges to very small amounts of food protein—as miniscule as the amount of peanut protein in half a peanut kernel—from peanuts, as well as two additional foods from a list including milk, eggs, wheat, cashews, hazelnuts, and walnuts.
At the end of the treatment, participants repeated the double-blind, placebo-controlled food challenges, but this time the goal doses of the food challenges were much higher. The results revealed that participants who had received omalizumab could tolerate much higher amounts of the allergens than those treated with placebo.
"After treatment, a majority of participants who reacted to the amount of milk protein in a teaspoon of milk were able to tolerate the amount of milk protein in a half of a cup," Mudd says. "Those who reacted to the tiniest bit of egg tolerated the amount of egg protein in half an egg. These are clinically relevant, significant amounts of food that demonstrate omalizumab's ability to protect patients from reacting to 'accidental ingestions.'"
Accidental ingestions were exactly what Joseph spent his childhood attempting to avoid. Turning family gatherings into minefields, Joseph's allergies also made his dream of visiting Egypt feel impossible. He hoped to one day travel there to experience his family's culture and enjoy the food.
After participating in CoFAR and discovering that omalizumab worked for him, Joseph, now 15, was able to realize that dream last summer.
"It brings tears to your eyes when you realize what this [medicine] means for families," Mudd says. "When we say it's life-changing, we really mean it."






