John Dempsey Hospital an 'Antimicrobial Stewardship Center of Excellence'
A commitment to responsible use of antibiotics earns UConn Health's John Dempsey Hospital the designation of "Antimicrobial Stewardship Center of Excellence" from the Infectious Diseases Society of America.
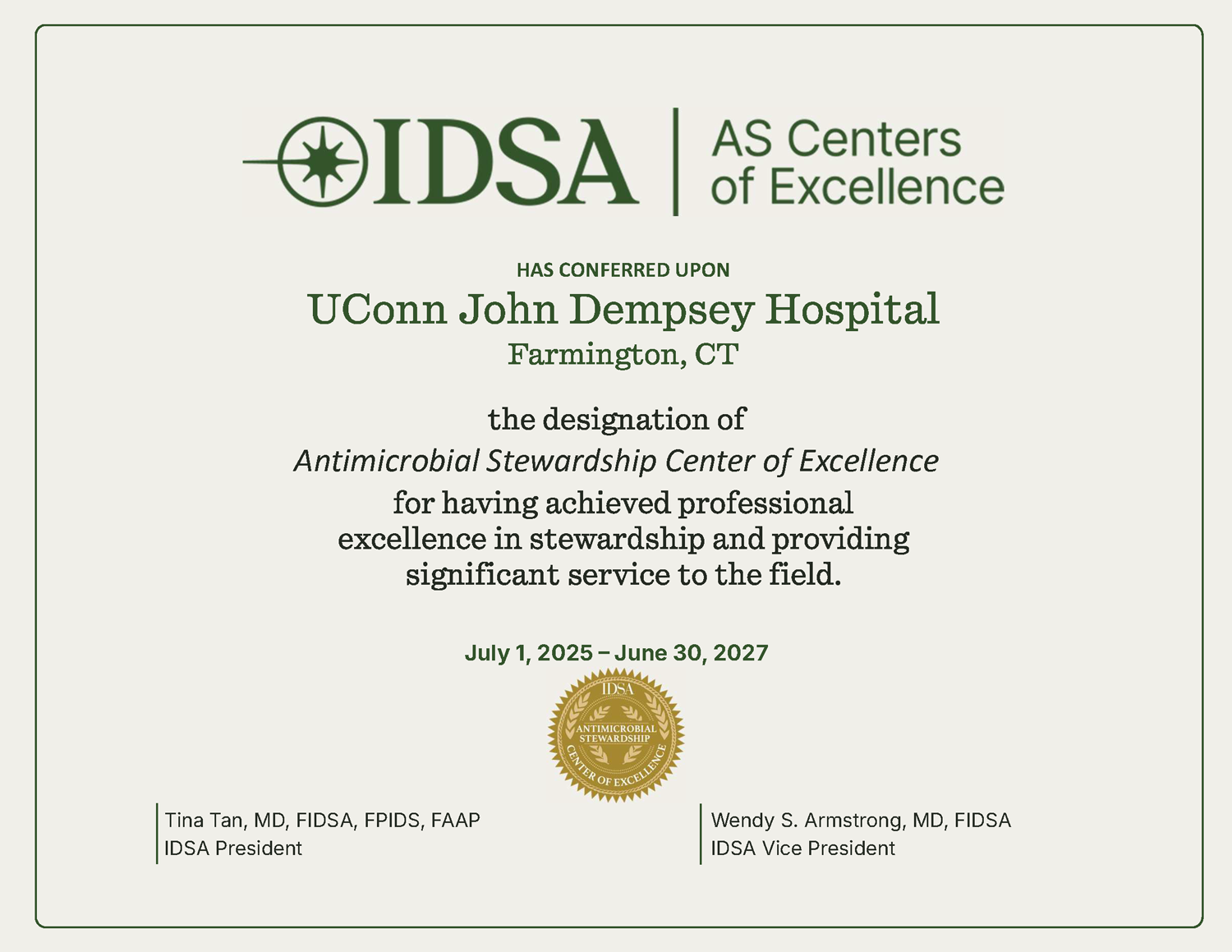
With this designation, the IDSA recognizes institutions that have established stewardship programs, led by infectious diseases physicians and pharmacists, to advance science in antimicrobial resistance, and that have surpassed high standards aligned with evidence-based national guidelines.
"Evolving antimicrobial resistance patterns and the introduction of new therapeutics have made antibiotic prescribing more challenging than ever," says Kevin Chamberlin, UConn Health's chief pharmacy officer. "This Center of Excellence designation is a testament to the sound antimicrobial stewardship we practice that protects our limited options for our most vulnerable patients."
John Dempsey Hospital is one of four hospitals in Connecticut designated as an Antimicrobial Stewardship Center of Excellence, and among fewer than 200 hospitals in the world that have earned the distinction since the ISDA started this program in 2017.
Core criteria include implementation of stewardship protocols by integrating best practices to slow the emergency of resistance, optimize the treatment of infections, reduce adverse events associated with antibiotic use, and address other challenging areas of antimicrobial stewardship.
"This shows that we are using multidisciplinary collaboration to ensure that we're using antibiotics in the most quality way and optimizing those antibiotics across care, both on the inpatient and outpatient side," says Gillian Kuszewski '03 (PHARM), '05 Pharm.D., university director of UConn Health's pharmacy residency programs.
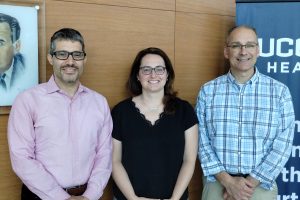
Kuszewski co-leads UConn Health's antibiotic stewardship program with Dr. David Banach '06 MD, MPH, infectious diseases physician and UConn Health's hospital epidemiologist, and Jeffrey Aeschlimann '93 (PHARM), a UConn School of Pharmacy faculty member and clinician in UConn Health's pharmacy practice.
"Antibiotic stewardship is a global health priority," Banach says. "The goal of using the right antibiotic for the right patient at the right time for the right duration is really becoming recognized as a key public health measure, both for reducing resistance and also reducing antibiotic-associated side effects and adverse events like C. diff."
C. diff, or Clostridioides difficile infection, is one of the most common health care-associated infections. It is highly contagious and difficult to treat.
"One of the important things the stewardship program does is minimize unnecessary use of broad-spectrum antibiotics, which has been shown to also decrease C. diff rates in hospitals and health care settings," Aeschlimann says.
While this is the first time UConn Health has applied for this ISDA designation, antimicrobial stewardship has been a priority going back more than a decade, predating regulatory requirements. Aeschlimann and Dr. Kevin Dieckhaus, who today is chief of UConn Health's Division of Infectious Diseases, started the antibiotic stewardship committee in 2013. Since then, it has grown to include representation from throughout the institution, including microbiology lab professionals, nurses, pharmacists, physicians, informatics specialists, infection preventionists, and students, residents and fellows.
"We've always been doing these things along the way, and we felt now was the right time to sit down and formally submit an application," Kuszewski says. "We've always done extremely well with our program when regulatory bodies like the Joint Commission come to visit. From a regulatory perspective, we've consistently received really good feedback from them on our antimicrobial stewardship activities."
She says the committee has established protocols, policies, and workflows to guide and support front-line providers in making the best choices.
"We've supported, for example, processes to make sure that even after the patient leaves the emergency department, they're on the right antibiotic based on follow-up information that we get from cultures," Kuszewski says.
"We have the collaborations between those who prescribe antibiotics and those who have expertise to offer and help support optimal prescribing," Banach says.
And the committee's guidance has made its way into the electronic health record system to provide an additional resource for prescribers.
"We try to develop either order sets or clinical pathways or popups, whatever we think might work best, to guide clinicians to pick the right antibiotic choice," Aeschlimann says.
Another strategy is to prioritize documentation of allergies to help inform prescribing decisions.
"They can choose an antibiotic with the least risk of a negative outcome," Kuszewski says. "Penicillin allergy documentation often leads to unnecessary use of certain antibiotics that come with greater risks. Perhaps a penicillin might cause some temporary stomach upset for a patient and is not really a true allergy. Clarifying this documentation in a patient's medical record can help providers determine which antibiotic carries the least risk in treating an infection."
Kuszewski notes that UConn Health leadership has been supportive of the antimicrobial stewardship efforts since the beginning.
"Not only are we following standards, but we're also seeing better outcomes," she says. "We also have results that show that we're using less broad-spectrum antibiotics than what we're expected to use, and our C. diff rates are down. The outcomes are actually tangible. It's not just what we say we're doing, but we're seeing good results."






