The vagus nerve has quietly shaped how our bodies function for thousands of years. Recently, it has moved into the spotlight, especially in wellness culture, where manipulating it is often described as a way to calm the body, reset the nervous system or even treat a wide range of conditions.
Author
- Arshad Majid
Professor of Cerebrovascular Neurology, School of Medicine and Population Health, University of Sheffield
As someone who researches the vagus nerve in clinical settings, I think it is important to explain what it actually does, what we know so far and where claims run ahead of the evidence.
The vagus nerve is one of 12 cranial nerves that emerge directly from the brain. It is the longest of them, extending from the brainstem through the neck and into the chest and abdomen. Along the way it connects to the heart, lungs, gastrointestinal tract and liver. You cannot see or feel it directly, but it helps regulate everything from your heartbeat to digestion.
Its name comes from the Latin word for "wanderer" , reflecting its long route through the body. One of the most important things to understand is that it is primarily a sensory nerve. Roughly 80% of its fibres carry information from the body back to the brain, acting as a constant internal monitoring system. Only about 20% of the fibres send signals from the brain to the organs.
In practice, this means the vagus nerve continually informs the brain about what is happening inside the body, including heart rate, digestion and inflammation.
Rest and digest
The vagus nerve is a major component of the autonomic nervous system, which controls functions we do not consciously regulate. This system has two main branches.
The sympathetic nervous system drives the fight-or-flight response . It increases heart rate, raises blood pressure and prepares the body for action.
The parasympathetic nervous system has the opposite effect. It slows the heart, supports digestion and promotes a calmer physiological state. The vagus nerve is the primary nerve of this system and is often described as supporting "rest and digest" functions .
This connection explains why the vagus nerve is linked to relaxation and stress regulation. But the relationship is often oversimplified in popular culture.
Many techniques promoted online, such as slow breathing, humming, singing or splashing cold water on the face, are said to stimulate the vagus nerve. These activities do not switch the vagus nerve on or off.
What these activities can do is indirectly influence vagal activity by signalling that the body is safe. Slow breathing with a long exhale, for example, can reduce heart rate and promote a calmer state. You might notice a slowing pulse or a general sense of settling.
In some people this effect is clear. In others it is minimal. Importantly, strong evidence on how reliably these techniques influence vagus nerve activity is still limited, and responses vary widely between people.
Medical vagus nerve stimulation
In clinical medicine, vagus nerve stimulation has been used for decades. There are two main approaches.
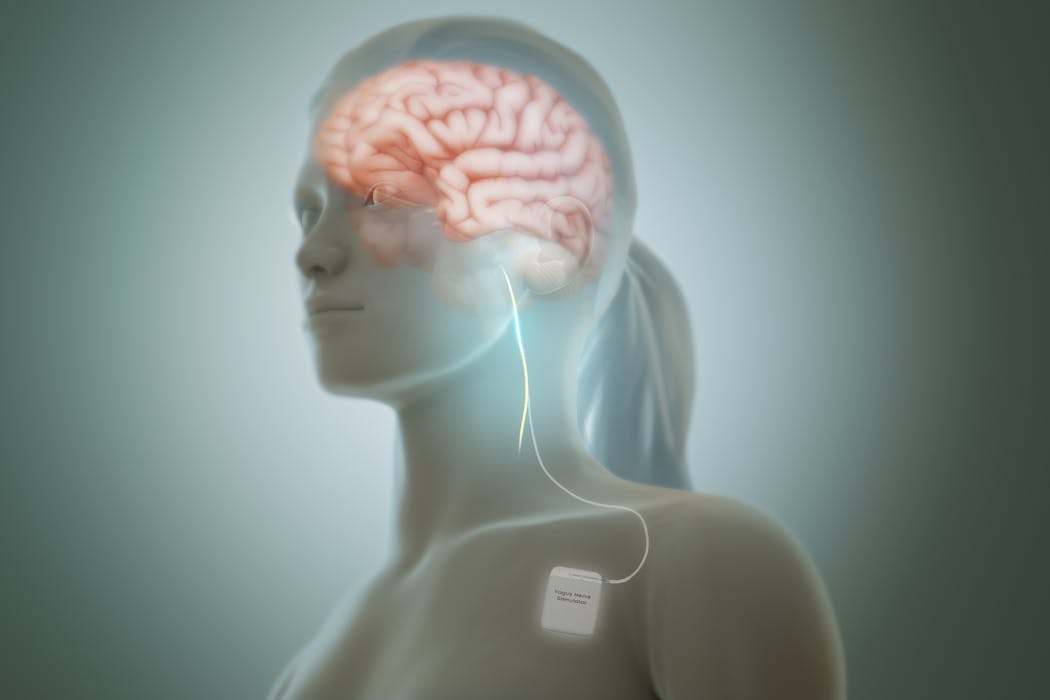
The first is invasive vagus nerve stimulation . This involves surgically implanting a small pacemaker-like device in the chest, with wires wrapped around the vagus nerve in the neck. The device delivers regular electrical stimulation directly to the nerve.
In the US, this treatment is approved for drug-resistant epilepsy and depression. It can be effective but is used less often in the UK because it requires surgery, ongoing care and significant cost .
The second approach, and the focus of much current research , is non-invasive vagus nerve stimulation. Studies show that a small branch of the vagus nerve supplies part of the outer ear . By placing electrodes on specific areas of the ear, researchers can stimulate this branch electrically without surgery.
Brain imaging studies suggest this produces patterns of activity similar to those seen with implanted devices. This gives researchers confidence that similar neural systems are being influenced , even if it is not always possible to confirm that only the vagus nerve is involved.
Medical vagus nerve stimulation devices must meet strict safety and evidence standards. They have to demonstrate clinical benefit in trials and continue to be monitored after approval .
Consumer wellness devices are not held to the same standards. Many can be sold without strong evidence that they stimulate the vagus nerve or improve health outcomes. This does not mean they are necessarily harmful, but claims about their effects should be treated cautiously.
Stroke recovery
One of the most promising areas of research is stroke rehabilitation. After a stroke, many patients experience weakness in one arm that can affect independence for years.
In ongoing research , my colleagues and I are investigating whether non-invasive vagus nerve stimulation, paired with physical rehabilitation, can improve arm function after stroke. The aim is to enhance neuroplasticity, the brain's ability to reorganise and form new connections, allowing healthy areas to take over lost functions.
This is being tested in a large clinical trial, in which neither participants nor researchers know who is receiving active stimulation until the end of the study. This helps reduce bias. If the results are positive, this approach could change how stroke rehabilitation is delivered.
Vagus nerve stimulation does not work the same for everyone. Some people experience headaches or worsening migraines. A small minority report changes in mood. In my own case, stimulation produces low mood, which is a recognised but uncommon response.
This variability is one reason why one-size-fits-all advice about stimulating the vagus nerve can be misleading.
The vagus nerve is not a cure-all. Most conditions involve multiple biological and psychological factors, and no single nerve explains or fixes them all.
It is, however, a crucial pathway linking the brain and body. As research progresses, we are likely to see more targeted, properly tested therapies using vagus nerve stimulation for specific conditions.
For now, the key message is caution without cynicism. The vagus nerve is real and important. The science is advancing. But meaningful benefits depend on careful research, appropriate use and an honest understanding of what the evidence does and does not yet show.
Strange Health is hosted by Katie Edwards and Dan Baumgardt. The executive producer is Gemma Ware, with video and sound editing for this episode by Anouk Millet. Artwork by Alice Mason.
In this episode, Dan and Katie talk about social media clips via TikTok from drjoedamiani , ayuswellness and prettyspatricia .
Listen to Strange Health via any of the apps listed above, download it directly via our RSS feed or find out how else to listen here . A transcript is available via the Apple Podcasts or Spotify apps.
![]()
Arshad Majid receives funding from the National Institute of Health research (NIHR) EME Programme for the TRICEPS trial which is investigating tVNS in stroke recovery.






