Over the past five years, medical anthropologist Annemarie Samuels has studied palliative care in different parts of the world. Over the next five years, she will focus on end-of-life care in the Netherlands. 'Everyone has the right to good care at the end of their life, but what that means differs from person to person.'
'What palliative care actually entails is a question on which opinions differ,' explains Annemarie. 'I would describe it as a professional form of care for people with very serious illness and towards the end of life. Although the illness does not have to be terminal for palliative care to be practiced, in most contexts around the world palliative care only comes into play in the final stage of life, sometimes even in the last few months or weeks,' she explains. 'Due to the enormous cultural diversity in the world, the concept of palliative care is changing: both how it is defined and how it is organised in practical and organisational terms. After all, everyone has a different idea of what a "good death" means.'

Learning from global contexts
Annemarie's research on global palliative care has also inspired her various research projects in the Netherlands. She sees a shift taking place in healthcare, with new medical technology and treatments presenting us with new dilemmas.
Annemarie has spent the last few years researching how palliative care is developing in different parts of the world, which has partly inspired her various research projects in the Netherlands. She sees a shift taking place in healthcare, with new medical technology and treatments presenting us with new dilemmas.
'On the one hand, there is enormous pressure from the pharmaceutical and medical industries to prolong life for as long as possible. On the other hand, there is a strong movement towards asking, ''Should we still be doing all of this?''. This is not only because of the costs, although that is often more difficult to discuss, but also because of the quality of life. Sometimes it harms people to undergo so many invasive life-prolonging treatments.' A positive development, Annemarie notes, is that doctors are increasingly coordinating their expectations and decisions with patients.
Ethnography to investigate what is not being said
Cooperation and good communication between doctor and patient are therefore important, but this can sometimes be difficult in practice. In some situations, patients do not want to know everything about their illness or prognosis, due to cultural or other factors.
But how do you conduct research on something that people would rather not talk about? 'Ethnographic research is ideal for this', explains Annemarie, 'precisely because it allows you to investigate what is not being said. There are many things you cannot ask with a questionnaire, because you will get a socially desirable answer, or because people are unable to articulate it. Think of things you can only observe and experience in practice, for example when you accompany someone to a doctor. Or when something is mentioned one time and not the next.'
''Ethnographic research is extremely well suited to this, precisely because it investigates what is not being said.''
Annemarie continues: 'As social scientists, we usually pay a lot of attention to what people say and less to what they don't say. In social science research, these silences are often approached from the perspective that something is taboo or that not talking about it is imposed from outside. However, there can be all kinds of conscious and unconscious reasons for not wanting to talk about something. Attention to not wanting to talk and not wanting to know also contrasts with the insistence on "open information provision" that is very common in the Netherlands and the rest of Europe.'
Interdisciplinary collaboration
This contrast is also something that doctors encounter. That is why Annemarie, together with colleagues from the Institute of Psychology in Leiden, researchers from Amsterdam UMC and the Pharos expertise centre, is developing a training programme for healthcare professionals to enable them to provide culturally sensitive care to people who do not need to know everything about their illness and prognosis.
'From a psychological perspective, there is a lot of knowledge about effective communication, about what is harmful to patients and what does help. Some useful techniques for this have also been developed', says Annemarie. 'It is very interesting to ask questions about this from an anthropological perspective, for example, what influence the different cultural and social backgrounds of both doctor and patient have on communication.'
A person is not merely their cultural background
But how do you develop a training programme that takes so many different experiences and contexts into account?
Annemarie emphasises that it is important not to essentialise a person's cultural or social background. 'People sometimes ask: '"If I am dealing with someone from a particular religious background, do I need to know everything about that religion in order to understand that person?". That is not necessary, because people are not defined by their religion or cultural background. These people can say something completely different from what someone else with the same religion or cultural background thinks or wants. It is therefore important to have an open and inquiring attitude.'
''It is therefore important to have an open and inquiring attitude.''
Making palliative care in Leiden more accessible
In addition to the training, Annemarie, together with health psychologist Liesbeth van Vliet and palliative care specialist Yvette van der Linden, recently carried out a smaller transdisciplinary project with various social partners in Leiden, both within palliative care and social welfare organisations. 'We wanted to bring all these parties together to see where we could start to make palliative care more accessible, especially for people who have difficulty connecting with institutions in society, a target group that is often difficult to reach.'
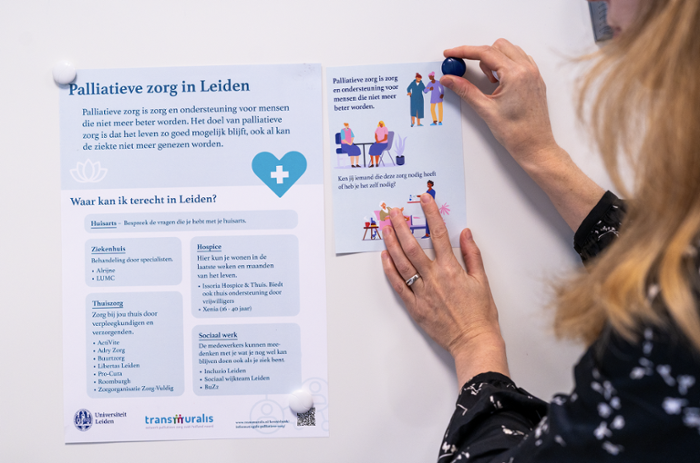
What makes it challenging is that palliative care can be a sensitive or even unfamiliar topic for some people, even though it can offer a great deal of support. 'Some people even think when they hear about palliative care: ''Oh, then they won't do anything for me anymore,'" says Annemarie. Together with all the partners, they created a flyer about where to go in Leiden for palliative care. Communication and language use are thus extremely important. To help healthcare professionals with this, Liesbeth and Annemarie have also developed another infographic in different languages. This infographic translates the important insights and tips developed by international experts in an accessible way and can therefore be applied directly in practice.
Ageing society
In addition to the new dilemmas arising from new medical technological developments, we are also dealing with an ageing society that is changing our view of healthcare. 'I notice that the questions I ask in my research are also being asked more often in public debate and are becoming increasingly pressing. In any case, I hope that the insights from my research projects can play a role in that debate.'
''The questions I ask in my research are being asked more frequently in public debate and are becoming increasingly pressing.''
More inclusive healthcare
Through her various research projects, Annemarie hopes to contribute to more inclusive healthcare: 'We cannot solve all social inequalities, but by gaining more insight into them and becoming more aware of them, we can try to ensure that more people receive healthcare that they themselves consider to be 'good". I don't know if that's too ambitious, but I certainly hope to be able to contribute to that.'
About Social Sciences Connect
Each month, we publish an article showcasing how social science research and education contribute to solving societal challenges. Researchers, lecturers, students, and societal partners work together to make knowledge accessible and to make a difference. Through open science and engaged education, we strengthen the connection between the university and society. In this way, we build a future together in which science and society go hand in hand.
Images by: Suédy Mauricio.
Text by: Sarah Bozuwa.






