A new boron agent drastically improves the effectiveness of boron neutron capture therapy for glioblastoma, demonstrate researchers at Tokyo Tech. The agent is selectively absorbed by brain tumor cells, exhibits enhanced blood retention, and can be administered at low doses. Experiments on cell cultures, mice, and rats show promising results, highlighting the potential of the novel agent for radiotherapy.
Glioblastoma (GBM) is a highly aggressive form of brain tumor that originates from supportive cells of the brain called glia. Due to its rapid growth, surgical removal of GBM is often difficult, leaving radiotherapy as the most viable option. Among the many existing radiotherapeutic modalities, boron neutron capture therapy (BNCT) has attracted a lot of attention for the treatment of GBM.
BNCT exploits the high affinity of boron-10 (10B) atoms for low-energy neutrons. When 10B absorbs a neutron, nuclear reactions release high-energy particles that damage the nearby biological tissue. Therefore, an essential requirement in BNCT is to achieve a significantly higher concentration of 10B in tumor cells than that in healthy normal cells. However, this has proven to be challenging, resulting in low survival rates and limited use of BNCT.
Against this backdrop, a research team including Professor Hiroyuki Nakamura from Tokyo Institute of Technology (Tokyo Tech) has developed a novel boron agent that shows great promise for BNCT. This molecule—pteroyl-closo-dodecaborate conjugated with a 4-(p-iodophenyl)butyric acid moiety (PBC-IP)—was thoroughly tested in their recent study published in the Journal of Controlled Release.
PBC-IP consists of three main functional groups (Figure 1): the first is a boron group containing twelve 10B atoms, the second is a ligand designed to bind to folate receptor α (FRα). This receptor, hardly present in normal cells, is greatly overexpressed in various cancers, including GBM. Thus, it acts as the entry point for PBC-IP into tumor cells. Finally, the third group is the 4-(p-iodophenyl)butyric acid moiety, which binds the entire molecule to albumin—an abundant carrier protein in blood that transports substances throughout the body. PBC-IP binds non-covalently to naturally present albumin, which allows it to directly interact with tumor cells, promoting its cellular uptake. Thus, the acid moiety can enhance the blood retention of the boron agent, thereby potentially reducing the required dose.
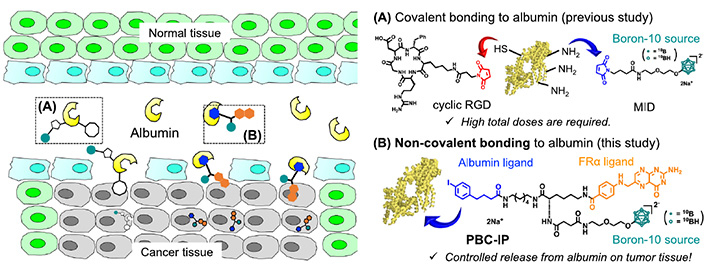
Figure 1. A new boron agent for the radiation-based treatment of glioblastoma.
(A) Previously studied and (B) proposed boron agents used to deliver boron to tumor cells. The way in which the new boron agent PBC-IP binds to the carrier protein albumin facilitates its accumulation in tumor cells even at low doses, leading to better treatment outcomes without toxic effects on healthy cells.
The researchers conducted several experiments to confirm the viability of PBC-IP for BNCT, finding that it accumulated in GBM cell cultures 10-20 times more than L-4-boronophenylalanine (BPA), a clinically approved boron agent in Japan. In addition, PBC-IP showed no signs of toxicity to cells on its own, demonstrating its safety. "Likewise, PBC-IP administrated intravenously to the human GBM xenograft model showed higher boron accumulation in tumors than BPA, effectively suppressing tumor growth after thermal neutron irradiation," highlights Prof. Nakamura.
These promising results were also replicated in vivo (Figure 2), both in GBM xenograft models and rat glioma models. PBC-IP administered via convection-enhanced delivery (CED) in the rat model achieved tumor-to-normal brain and tumor-to-blood boron ratios of 37.8 and 94.6, respectively, three hours after completion of CED. "Survival rates at 180 days were 50% and 70% following BNCT with PBC-IP only and PBC-IP in combination with BPA, respectively. There were no residual brain tumors," says an excited Prof. Nakamura.
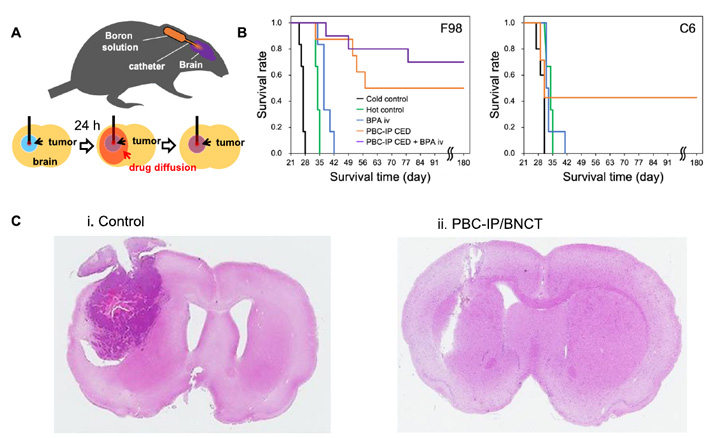
Figure 2. PBC-IP greatly increases the survival rate in rats with glioma.
(A) Schematic image of CED method. (B) Kaplan-Meier survival curves for F98 and C6 glioma rats after thermal neutron irradiation. (C) Hematoxylin- and eosin-stained sections of F98 glioma brains obtained from rats with irradiation only (i. control) and rats surviving for 180 days after BNCT with PBC-IP/CED (ii. PBC-IP/BNCT).
Overall, the proposed boron agent may represent a breakthrough in radiotherapy for GBM, with the researchers currently conducting preclinical studies.
Let us hope that their efforts would lead to better tools for fighting GBM and other cancers!
Reference
Authors : |
Kai Nishimura1, Hideki Kashiwagi2, Taiki Morita1,3, Yusuke Fukuo2, Satoshi Okada1,3, Kazuki Miura1,3, Yoshitaka Matsumoto4, Yu Sugawara4, Takayuki Enomoto5, Minoru Suzuki6, Kei Nakai4, Shinji Kawabata2, and Hiroyuki Nakamura1,3
|
Title : |
Efficient neutron capture therapy of glioblastoma with pteroyl-closo-dodecaborate-conjugated 4-(p-iodophenyl)butyric acid (PBC-IP) |
Journal : |
Journal of Controlled Release |
DOI : |
|
Affiliations : |
1School of Life Science and Technology, Tokyo Institute of Technology
2Department of Neurosurgery, Osaka Medical and Pharmaceutical University 3Laboratory for Chemistry and Life Science, Institute of Innovative Research, Tokyo Institute of Technology 4Department of Radiation Oncology, Faculty of Medicine, University of Tsukuba 5Biomaterials Analysis Division, Open Facility Center, Tokyo Institute of Technology 6Institute for Integrated Radiation and Nuclear Science, Kyoto University |






