Nearly $6.8 million in new federal grants will enable researchers to collaborate with agencies across the state, including the Rhode Island Department of Health, to investigate innovative ways to tackle the opioid crisis.
PROVIDENCE, R.I. [Brown University] - With opioid drug overdose deaths skyrocketing in recent decades, researchers at Brown University's School of Public Health are confronting the epidemic in multiple ways. Two new five-year grants from the National Institutes of Health, totaling $6.8 million, will expand those efforts.
The first will launch a partnership with the State of Rhode Island that will result in neighborhood-based intervention strategies across the state's cities and towns informed by a new predictive forecasting model. The second will enable researchers to evaluate the effectiveness of test strips used to detect fentanyl, a highly potent prescription opioid often used to lace other heroin or cocaine, but hard for drug users to detect.
"Both projects are trying to bring innovative technologies to help solve the overdose crisis," said Brandon Marshall, an associate professor of epidemiology at Brown and principal investigator for both projects. "That's the long-term goal - to reduce the risk of overdose and to save lives."
The first project - titled Preventing Overdose Using Information and Data from the Environment (PROVIDENT) - expands on several years of collaboration among Brown researchers and agencies across Rhode Island.
PROVIDENT will unite Brown scholars with colleagues from NYU School of Medicine (Magdalena Cerdá, associate professor of population health, is co-principal investigator) and the University of California, Berkeley, to develop a machine-learning forecasting model to predict which neighborhoods in Rhode Island are most at risk for outbreaks of opioid overdose.

Next, the Brown team will work with the Rhode Island Department of Health (RIDOH) to test whether the model's predictions can help deliver interventions - peer recovery coaching, opioid agonist therapy or naloxone distribution - specifically to neighborhoods that would benefit most. In a randomized trial, half of the state's 39 cities and towns will be assigned PROVIDENT model predictions that will guide RIDOH's distribution of resources, while the other half will receive interventions without the targeting of particular neighborhoods.
"We hope that in towns where we develop the predictions, we'll see a 40% reduction in all overdoses, fatal and nonfatal," Marshall said. "That's an ambitious target. But we think we can get there by working collaboratively across the state and with organizations that deliver services."
Dr. Nicole Alexander-Scott, RIDOH director and an associate professor at Brown, said the state/university partnership is illustrative of the collaborative approach that often leads to the most innovative solutions to public health challenges.
"This research partnership between the talented public health professionals throughout RIDOH who are responding to the overdose epidemic and the Brown University School of Public Health, with support from the RIDOH Academic Institute, represents a cutting-edge intervention to get tools and resources related to substance-use disorder into the communities where they are needed most," Alexander said. "By synchronizing existing statewide overdose surveillance systems with powerful predictive analytics and data forecast tools, we will be leveraging data in powerful new ways to prevent overdoses and safe lives. Saving lives remains our absolute priority in this crisis."
Marshall, an expert adviser to Rhode Island Gov. Gina Raimondo's Overdose Prevention and Intervention Task Force, said that if the trial proves successful, the research team's long-term goal is to ultimately expand the use of the model beyond the Ocean State.
"Rhode Island is a perfect laboratory for this particular project, to see whether we can successfully predict overdoses at a neighborhood level," Marshall said. "If we can, then the next steps would be disseminating the forecasting tool to other states and evaluating whether it's useful in other contexts."
The second NIH grant, which will fund a project titled Rhode Island Prescription and Illicit Drug Study (RAPIDS), will address a very different facet of the opioid crisis - fentanyl. The highly potent synthetic opioid can be deadly even in trace amounts and is a major factor in the rise in fatal overdoses.
"Fentanyl is about 50 to 100 times more powerful than heroin or morphine, and it's cut into the illicit drug supply," Marshall said. "Essentially, people can't find pure heroin on the East Coast - nowadays, it's all adulterated with fentanyl. In the last couple of years, we've seen evidence that it may be appearing in other types of illicit drugs as well."
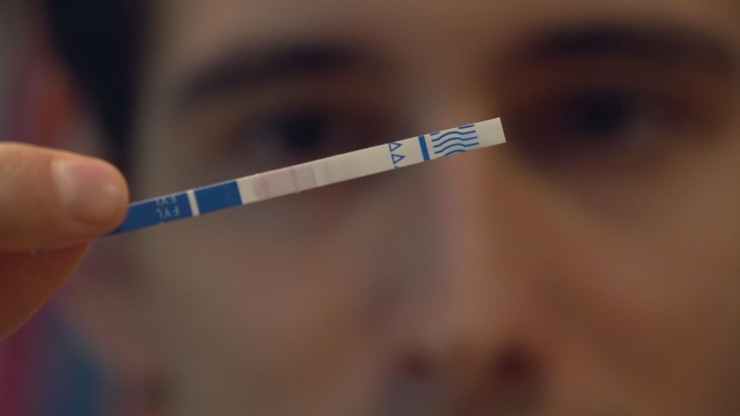
About five years ago, fentanyl test strips became available. Originally developed for urine drug screens, the rapid-acting strips have increasingly been used to detect the presence of fentanyl in illicit drugs. They work essentially like over-the-counter pregnancy tests. Each single-use strip is dipped into water containing a bit of drug residue, and after a minute, either one or two red lines appear - one line means the liquid contains fentanyl, and two lines means the test did not detect the drug.
The RAPIDS project will consist of a randomized trial that includes individuals who use drugs and are at risk for fentanyl overdoses. The project will test whether informing people about the dangers of fentanyl and teaching them to use the strips reduces risk of overdose. Marshall said he expects the trial to launch in December 2019, and the research team hypothesizes that the test-strips will lower overdose rates.
"The hope is that people at risk for fentanyl overdose will use these strips, like them and take actions that meaningfully reduce their risk," Marshall said. "I'm optimistic that we will see those reductions."
The project will expand significantly on the results of a 2018 pilot study led by Marshall. The study provided test strips to 93 young adults who reported injecting opioids or using heroin, cocaine or prescription pills bought off the streets. The preliminary results were promising.
If the expanded trial indicates that strips can decrease overdose rates, Marshall and his colleagues will next evaluate the extent to which they're disseminated, and how. Participant safety is a top concern, he added.
"There are other adulterants out there that increase the risk of overdose that the strips don't detect, including some fentanyl analogs," he said. "So the strips aren't perfect, and we're focusing on how to communicate that to participants - to let them know that they should take universal precautions whenever they use an illicit substance, like not using alone and having someone there who could call 911 in the event of an overdose."
National Institutes of Health funding for PROVIDENT (No. R01DA046620) is expected to total $3.3 million over five years. NIH funding for RAPIDS (No. R01DA047975) is expected to total $3.5 million over five years.
This news story was authored by contributing science writer Kerry Benson.