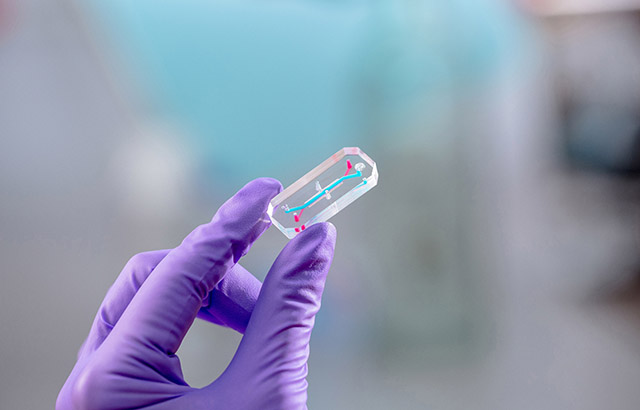
Bioengineers at Queen Mary University of London have taken a significant step forward in the development of laboratory-based models of human tissues which may be used as alternatives to animal testing. The group develops organ-on-a-chip technology in which human cells are grown in tiny plastic 'chips' to mimic the biology of tissues found in the body. In their latest research, published in the Journal of Tissue Engineering, the group describes new methods to increase the complexity of these models, making them even more like human tissues.
The study offers a new way to precisely guide cell behaviour by controlling the spatial distribution of growth factors, which act as biological signalling molecules. By doing so, the team was able to recreate different tissues in different locations, mimicking the interfaces between tissues which are critical in both health and disease.
"The tissues in our bodies are incredibly complex, and recreating this complexity in the laboratory is difficult, said Dr Tim Hopkins, the lead researcher in the study. "Techniques such as organ-on-a-chip offer an improved option to generate tissue models but, until now, methods to really mimic tissue complexity in these models were lacking. By creating gradients of growth factors, we can recreate the complex environment that cells experience in the body, so that they behave in the same way in our models."
What makes this breakthrough especially exciting is that the new methods work across a range of different human tissues and different commercial platforms. This means that the research can be used to help scientists understand disease processes and test new therapies, across a wide range of human diseases, without the use of animals which often poorly predict human biology.
"This work could make a big difference to how we study diseases and test drugs, said Professor Martin Knight, Co-Director of Queen Mary's Centre for Predictive in vitro Models. "This research could help speed up the development of safer, more effective treatments, and reduce our reliance on animal testing."
To demonstrate the capability of these new methods, Professor Knight, Dr Hopkins and the team used a growth factor called bone morphogenetic protein-2 (BMP-2) which is heavily involved in bone development. By creating regions in the organ-chips with high and low concentrations of BMP-2, the researchers could control the behaviour of human stem cells within the system, generating bone-like regions interfacing with cartilage-like regions, and mimicking the natural process of bone development.
The work was funded by grants from the National Centre for Replacement, Reduction and Refinement of animals in research (NC3Rs), the Biotechnology and Biological Sciences Research Council (BBSRC) and the Engineering and Physical Sciences Research Council (EPSRC). The team are working on a range of organ-on-a-chip technology, developing and validating new techniques and models of different organs and diseases, in partnership with industry.






