Oregon Health & Science University is part of a new international initiative harnessing artificial intelligence to develop and enhance lab-grown systems, such as "organs-on-a-chip," to improve understanding of disease and accelerate new medications.
The overall £15.9 million initiative — more than $18.4 million — is jointly funded by the Medical Research Council, Wellcome and Innovate UK. It is based in the United Kingdom, and includes arms of research covering the liver, brain, cancer, pain and blood vessels.
"OHSU is proud to be part of this new initiative that leverages the promise of artificial intelligence to advance the health of people here in Oregon and around the world," said university President Shereef Elnahal, M.D., M.B.A. "Decades from now, we will look back at this era as an inflection point in the advancement of new tools to improve treatment of disease."

The OHSU portion involves the study of blood vessels and is led by Owen McCarty, Ph.D., Gordon Moore Endowed Chair of biomedical engineering in the OHSU School of Medicine.
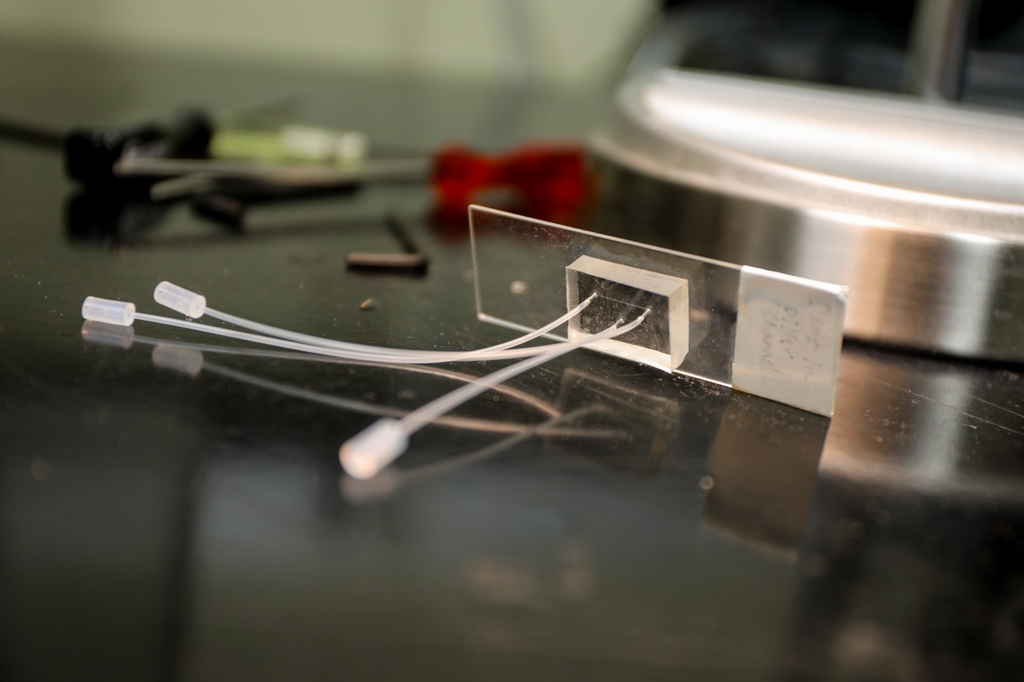
McCarty, a chemical engineer by training, will lead the work at OHSU in tandem with the Hull York Medical School in the U.K. to develop lab-grown, artificial blood vessels, replicating key aspects of the human circulatory system, such as blood flow, vessel structure and clot formation.
"Right now, there is just not a good model for bleeding," McCarty said. "One of the goals of this project is to study not just blood in circulation, but also to study the vessel wall."
Over the coming decades, McCarty expects these new approach methodologies will improve existing animal models and reduce — and someday eliminate — the use of animal models altogether.
By developing scalable, adaptable artificial blood vessels, the international team of researchers expects to replicate key aspects of the human circulation system. The goal is to accelerate effective treatments for cardiovascular disease, which accounts for almost a third of global mortality — with great majority of those deaths associated with blood clots in the heart, in the form of heart attacks, or the brain, in the form of stroke.
"Our goal is to build reliable, non-animal methods that are fit for modern drug discovery," said Simon Calaminus, Ph.D., the principal investigator with Hull York Medical School in the U.K.
McCarty pointed out that blood itself is a critical organ in the body — distributing oxygen, surveying for infection or inflammation, picking up debris and cleaning it through the kidneys.
Yet, millions of people worldwide suffer from the effect of blood clots.
"The goal is to make sure blood doesn't clot in diseased vessels but also doesn't leak out in the form of bleeding," McCarty said. "Safe drugs to prevent heart attack and stroke must walk this biological tightrope."
McCarty and colleagues in the U.K. will attempt to answer the question through one of five projects being funded in the initiative: ARTEMIS — ARTificial blood vessels for Thrombosis, Endothelial Modeling and artificial intelligence Simulation.






