Katie Hunter sensed a problem while giving birth to her second son, Ryder.
"I had a feeling something was wrong when I started pushing," recalled Katie. "Giving birth to my first child had been so smooth and easy, but with Ryder something just did not feel right."

Katie and her husband Dan Nunes grew even more worried right after delivery, as Ryder was gasping for air. The medical staff tried multiple times to keep the baby's upper airway open to no avail. The team then intubated Ryder and sent him from South Lake Tahoe to UC Davis Medical Center in Sacramento.
"I only got to be with him for a few minutes before he was transported to UC Davis," shared Katie. "I felt frozen and numb — I didn't know what was happening and thought we might lose our child."
Ryder was diagnosed with Robin sequence, a rare condition in which an infant has a smaller than normal lower jaw and a tongue that falls back in the throat. One out of every 8,500 to 14,000 babies are born with the condition, which had gone undiscovered through Katie's entire pregnancy.
Robin sequence can cause an infant's tongue to be pushed far back in the throat, prompting severe trouble breathing and swallowing without assistance. In severe cases, an infant will need a tracheostomy, a life-saving procedure where a surgeon opens a hole in the patient's neck and connects a tube for unimpeded breathing.
Parents face a difficult choice
At UC Davis Health, Katie and Dan met with Ryder's care team, which included Alex Marston, a pediatric head and neck surgeon, and surgeon on the multidisciplinary UC Davis Cleft and Craniofacial team.
Despite the care team's best efforts, Ryder was still unable to breathe on his own or feed well. In addition, he had self-extubated, or removed the endotracheal airway tube helping him breathe, multiple times.
The care team presented Katie and Dan with two treatment options.
The first included giving Ryder a tracheostomy to help him breathe and attaching a gastrostomy tube into his belly to provide much-needed nutrition.
"A tracheostomy and gastrostomy tube do help with breathing and feeding, but they are both temporary solutions and present other challenges," explained Marston. "A tracheostomy usually remains in place for a few years, requires specialized nursing care and can lead to delays in eating, drinking and speech and language development."
The other treatment option was a procedure called mandibular distraction surgery, which has been offered at UC Davis Health for over 20 years.
"Mandibular distraction is a procedure done for infants with Robin sequence that lengthens the jaw to help open the airway so the baby can breathe and feed safely on their own. It is a specialized surgery, but it provides a more long-lasting solution for the condition."-Alex Marston
"Mandibular distraction is a procedure done for infants with Robin sequence that lengthens the jaw to help open the airway so the baby can breathe and feed safely on their own," Marston said. "It is a specialized surgery, but it provides a more long-lasting solution for the condition."
After many conversations, Katie and Dan decided Ryder would undergo a mandibular distraction.
"Dr. Marston and the entire team were so patient and supportive of us," recalled Katie. "We asked a lot of questions, and they took their time to clearly explain all the details we needed to make an informed decision."
Mandibular distraction surgery
To prepare for the procedure, Marston and his team utilized a new technology called augmented reality, which is being used by some UC Davis Health surgeons.
Through augmented reality goggles, surgeons can project 3D computed tomography (CT) and MRI scans that overlay critical information directly into their field of view. The goggles help them:
- Envision and plan the surgical approach
- Visualize hidden vascular, nerve and bone structures
- Localize instrumentation and implants
- Project drilling and cutting guides
"The goggles allow us to better transition our virtual surgical plans to the operating room," said Marston. "During surgery we have a better idea of the patient's anatomy and can visualize objects that otherwise would be very difficult to see in a precise manner."
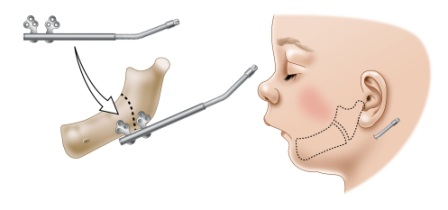
During the procedure, surgeons made a small incision under Ryder's jaw on both sides of his neck. They cut his mandibular bone, commonly known as the lower jaw, on both sides to separate the front and back of the jaw.
The team placed two distraction devices on each side and attached them with pins to the front and back sections of the bone. Small activation arms were then connected to the distraction devices so that they could be turned and widen the cut mandibular bones.
A few days after surgery, the team maneuvered the activation arms to slowly move Ryder's jaw forward, widening the space between the cut edges of the bone and allowing new bone to form in the space.
"The distraction procedure makes the jaw longer and also improves the position of the tongue," explained Marston. "By doing so, we create more space in the airway, which allows the infant to be able to breathe on their own and feed better."
Back on track
Following the complex procedure, doctors removed Ryder's ventilator tube. Ryder transitioned to a CPAP (continuous positive airway pressure) machine and then to a nasal cannula, a thin tube that provides additional oxygen through the nose.
Just two weeks later, after spending 66 days in the UC Davis Health Neonatal Intensive Care Unit, Ryder was discharged and traveled home to South Lake Tahoe.
His parents were thrilled with Ryder's care.
"We have the utmost gratitude for the UC Davis care team, they gave our child a chance to live a normal life," Katie shared.
Today, Ryder is all smiles. Despite his challenges he is back on track with development goals.
"He is just the happiest little guy," reflected Katie. "He truly is a miracle baby."







