UConn neuroscientist and chemist receive NIH R01 grant to support their collaboration
In an ischemic stroke (the most common type), blood flow is blocked to a portion of the brain, depriving it of oxygen. This causes the immediate, recognizable symptoms of stroke: muscle weakness on one side of the body or face, slurred speech, and loss of balance.
But the brain damage that occurs from this lack of oxygen isn't temporary - it causes a cascading effect of inflammation and tissue damage within the brain. This is why stroke is a leading cause of long-term disability worldwide. Chronic consequences can include paralysis, memory loss, and depression.
If there were a drug that could interrupt this process, it could effectively "turn back time" for patients after stroke. Two UConn researchers are one step closer to developing this medication, after receiving a $2.6 million R01 grant for five years from the National Institutes of Health (NIH).
"The only current FDA-approved drug for stroke is the 'clot-buster' drug" known as tPA, explains Rajkumar Verma, Ph.D. "It's approved only if you are able to deliver this drug within 4.5 hours of the stroke onset. Approximately ninety percent of stroke patients are ineligible for this treatment, because either they are outside this treatment window or do not qualify due to various reasons such as age, medical history, etc."
Verma, an assistant professor in the Departments of Neuroscience and Neurosurgery at UConn School of Medicine, saw this as a huge unmet need.
A Cross-Campus Collaboration
Verma teamed up with Raman Bahal, Ph.D., an associate professor in the UConn School of Pharmacy. Bahal's expertise in chemistry and drug delivery has earned him honors from the National Academy of Medicine and the National Academy of Inventors.
But Verma knew him from a more casual context: on the cricket pitch in New Haven, where they met while Bahal was working at Yale University. Through gametime conversations about work, Verma realized that Bahal's research group produced the very same molecules he was investigating for their potential in treating stroke.

For his part, Bahal has worked in the field of nucleic acid chemistry since graduate school; but he always felt that "if we don't get a complementary collaborator who can do biology, then it's an unfinished story."
Now, working in Farmington and Storrs (respectively), Verma and Bahal are combining their unique perspectives on stroke biology and drug chemistry in a methodical search for a cure.
"We are longtime friends, and we're always discussing ideas together," Bahal says. "On this collaboration, we work in synergy - if Dr. Verma needs a molecule, my lab will make it, and his will be ready to test it."
Their efforts were first recognized with a Research Excellence Program (REP) grant from UConn's Office of the Vice President for Research. Then, they received an NIH R21 grant to further explore and develop their concept. Results were published in 2024 in the journal Molecular Therapy: Nucleic Acid.
With this latest R01 award, the pair will begin testing variations of the base molecule they previously developed - aiming to create even more effective analogs.
"The whole idea is figuring out how we can deliver it in the safest and most effective way possible," says Bahal.
Stopping the Clock
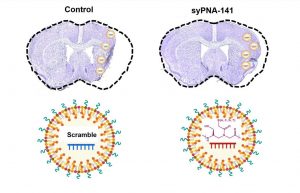
The therapy in development by Verma and Bahal is called an miRNA inhibitor. It works by targeting "micro-RNAs," small molecules that regulate protein expression inside cells.
UConn researchers discovered that during a stroke, these miRNAs get dysregulated, thus leading to brain damage by multiple unchecked proteins, according to Verma. An miRNA inhibitor medication can keep this damage in check. In mouse models, it has already proven effective at restoring motor function and memory after ischemic stroke.
When used in human patients down the road, the medication could be administered in a hospital setting in an injection or infusion form.
"Every minute matters in treating stroke," says Verma. "Timing is very critical. However, our goal with this drug is to extend this window significantly and see if we can still get neuroprotection."
Another notable benefit of this treatment is that it would require only one dose. If successful and approved, a single injection of this miRNA inhibitor would be sufficient for neuroprotection up to 15 days after stroke. This means it would be logistically easier to administer, as well as safer: there is a much lower chance of a patient having an adverse reaction to the drug if it is only given once.
Verma notes that the brain is a notoriously tricky organ to medicate, due to the blood-brain barrier which serves to insulate the brain from toxins in the bloodstream — and also filters out many drug molecules.
However, "during a stroke, there is a natural blood-brain barrier opening for up to seven days, so that gives an advantage for the therapy to be able to go into the brain," Verma says. "In the future, we'd like to develop a formulation that will work for more long-term treatment even when the blood-brain barrier is closed, or partially closed, during the recovery phase."
Verma and Bahal are working with UConn's Technology Commercialization Services (TCS) team to connect with companies to market their molecules. Verma also presented this innovation at UConn Health's inaugural Innovation Catalyst event on July 23 to industry and investors.
Right now, they have a patent pending for the original molecule they developed and are in talks with several interested companies who may later develop the promising stroke therapy candidates.
"If we are successful in making this drug," says Verma, "it is going to change the field forever."






