
When it comes to questions about fungal infections, Andrej Spec, MD, has become the go-to expert for doctors around the world. Each week, he takes 10 to 15 calls from physicians struggling with complex fungal diagnosis or treatment questions. He has fielded queries from all across the U.S. and as far away as China, Thailand, Japan, Australia and Europe.
"The problem is that many doctors were trained to think of fungal infections as regional and rare," said Spec, an associate professor of medicine in the Division of Infectious Diseases. "So when patients come in with signs of an infection, they don't consider that it might be a fungus until everything else has failed."
This medical blind spot can send patients with fungal infections on long and frustrating diagnostic odysseys that prolong illnesses and worsen outcomes. The WashU Medicine Invasive Fungal Infections Clinic, launched in 2015, is making great strides to shorten that odyssey and provide world-class diagnosis and care for this often-overlooked class of infectious diseases. In its first decade, the clinic has grown from a single specialist seeing three or four patients a week to a busy practice with three physicians, 1,200 patient visits a year and an international reputation that has drawn patients from 37 U.S. states and five countries. Last year, the clinic was named a Center of Excellence, Diamond Level, by the European Confederation of Medical Mycology. It is one of only 13 clinics in the world to achieve this distinction and one of only two in the U.S. The other is at MD Anderson Cancer Center and only treats MD Anderson patients; it doesn't take referrals.
"It's not easy to earn this recognition," said Spec, the founding director of the WashU Medicine fungal clinic. "You have to demonstrate excellence in three areas: diagnosis and testing; patient care; and research. Patients come here when they run out of options at other places."
Surviving scopulariopsis

St. Louis resident Jonathan Ferretti, now 22, counts himself lucky that the WashU Medicine fungal clinic was nearby when he contracted one of the rarest and most lethal fungal infections. In 2020, he was undergoing treatment for an aggressive leukemia at St. Louis Children's Hospital when black spots started appearing on his body, first on his knee, then his back. Successfully treating Ferretti's leukemia involved targeting the same immune cells that fight off infections, and the black spots immediately caught the attention of Ferretti's care team, including WashU Medicine pediatric oncologist Shalini Shenoy, MD, and WashU Medicine pediatric infectious disease specialist Rachel Orscheln, MD. Both doctors are professors of pediatrics who treat patients at St. Louis Children's Hospital.
They called in Spec to evaluate the patient, and he made the diagnosis: the spots were caused by Scopulariopsis, a soil fungus that had taken advantage of Ferretti's ravaged immune system to invade his bloodstream and spread throughout his body.
At the time, only a few dozen cases of disseminated scopulariopsis disease - meaning, disease that had spread throughout the body - had been reported in the medical literature. All had been fatal.
"By the time I got scopulariopsis, I had been through chemo, radiation, intubation and a stem-cell transplant for leukemia," Ferretti said. "My thought process had gotten so distorted by cancer treatment that I didn't realize how bad this fungus was. I thought it was just one more thing I had to deal with."
Before Ferretti began intensive cancer treatment, his doctors had prescribed, as a precaution, three of the best anti-fungal medications to keep such infections at bay but none was effective against the scopulariopsis taking over his body. With no treatments approved by the Food and Drug Administration (FDA) specifically for disseminated scopulariopsis and the infection spreading rapidly, Spec recognized that Ferretti's only chance of survival was a clinical trial for the experimental antifungal agent olorofim, made by the biotech company F2G. Spec and his team rushed to get Ferretti enrolled in the trial and on the drug.
Within weeks, the spots began to disappear, although it was more than a year before Spec felt comfortable taking Ferretti off the drug. The trial has since concluded, and F2G is in the process of applying to the FDA for approval for olorofim.
"When Dr. Spec told me that I may have been the first person to survive disseminated scopulariopsis, I was shocked," Ferretti said. "I still can't believe it."
Expanding expertise beyond WashU Medicine
Ferretti is one of thousands of patients whose lives have been changed by the Invasive Fungal Infections Clinic. The clinic has built its reputation on providing advanced diagnostics and leading-edge treatment for all kinds of fungal infections, but its specialty is Histoplasma, a soil fungus that causes histoplasmosis, an infection with flu-like symptoms such as fever, cough and chills. But histoplasmosis is much deadlier than the flu. Overall, the fungus kills about 5% of people who contract it, and the death rate rises to 30% or more for people with compromised immune systems.
The mold occurs worldwide but its global hotspot is right here in the Midwest, and WashU Medicine physicians and researchers have developed internationally recognized expertise in diagnosing and treating histoplasmosis. The WashU Medicine clinic also boasts what is possibly the only multidisciplinary care team specializing in a rare but serious and lifelong complication of histoplasmosis called fibrosing mediastinitis. In this condition, abnormal growth of tissues in the chest can lead to blockages of airways, blood vessels and the esophagus.
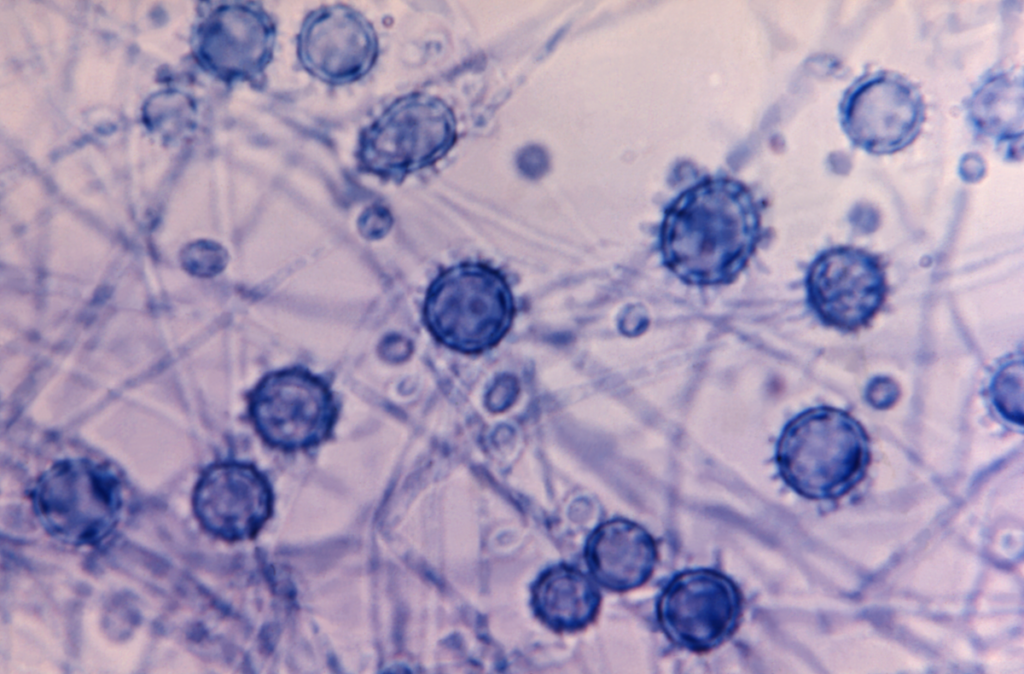
In addition, the clinic is participating in several clinical trials for other fungal infections. Such trials can provide access to experimental medications for people who have exhausted approved alternatives. The clinic's physicians also conduct research on fungal infections, with a focus on Cryptococcus, Histoplasma, Candida, Aspergillus and other invasive molds, including the epidemiology of such infections and factors that affect outcomes in patients infected.
Most people with invasive fungal infections experience at least one incorrect diagnosis and unhelpful treatment; nationwide, the median number of misdiagnoses among fungal infection patients is four. Adriana Rauseo, MD, an assistant professor of medicine and a member of the clinical faculty at the fungal clinic, is working on shortening the diagnostic journey for patients by educating primary-care providers on identifying fungal infections.
"If we're going to bring down the number of misdiagnoses, we need to increase awareness of fungal infections beyond infectious diseases specialists," Rauseo said. "We need primary-care providers to start to 'think fungi.' I don't know if it's realistic to get to the point where people are diagnosed, on average, on the first try. But being diagnosed the second time you go to the doctor is much better than the fifth. The plan is to start with local providers and then expand further afield."
Because it houses the fungal clinic, WashU Medicine is one of the few places that can provide intensive training in diagnosing and treating invasive fungal infections. Infectious disease fellows at other institutions sometimes do a rotation at WashU Medicine specifically so they can train in the fungal clinic.
The medical community needs to get up to speed on fungi quickly because things may be worsening. A 2022 paper by Spec and colleagues showed that lung infections caused by environmental fungi - once restricted to certain areas of the U.S. - have become a problem nationwide because some species of pathogenic fungi have expanded out of their traditional ranges in recent decades, possibly driven by climate change.
Worse, new fungal pathogens are poised to emerge, Spec adds. Many fungi that live in the soil, water and air have all the molecular tools to cause disease in people but rarely do, primarily because they are adapted for cooler temperatures and don't fare well at human body temperature. But with a warming climate driving longer and hotter heat waves, environmental fungi are under pressure to adapt to higher temperatures. Fungi may break bad in a warmer world.
Patient collaborations improve care
Patrick B. Mazi, MD, an assistant professor of medicine and the third member of the fungal clinic faculty, sits on the board of the fungal patient advocacy group Mycology Advocacy, Research & Education, or MyCARE. Co-founded by Spec in 2023 with Rob Purdie, a patient activist, and Lisa Tushla, a medical education professional, MyCARE aims to improve diagnosis and treatment of fungal infections by raising awareness, supporting patients and caregivers and advocating for more and better research.
"Rob Purdie likes to say, 'I was diagnosed with a 50-year-old test and am being treated with a 70-year-old medication. In no other medical diagnosis would that sentence be acceptable,'" Mazi said. "He's right! If we are going to get a handle on invasive fungal infections, we need better diagnostics and better treatments, and that means research."
Clinical mycology, the scientific study and treatment of fungal infections, is vastly underfunded compared to other disease areas, so fungal researchers have to get creative. They are turning to patients such as Purdie to help guide research in the directions that will have the biggest impact on patients' lives.
"I have to admit that I was a bit surprised when I first spoke to patients and caregivers about their priorities," Mazi said. "I was guilty of assuming that better treatments would be at the top of everyone's list. But most of the patients advocate for improved diagnostics so that they could have been diagnosed and treated more quickly. What that told me was that their experience with the early part of their fungal infection journey was so unpleasant that even years later they would prefer to fix that for patients that come after them over finding better treatments for themselves."
Today, Ferretti is a mostly healthy 22-year-old college student with plans to go into pediatric oncology nursing. There are still some lingering effects of his cancer treatment, but he has recovered fully from his bout with one of the deadliest fungi in the world. He and his mother attended MyCARE's first meeting in May 2023 in Denver, where one of the co-founders is based.
"This conference opened my eyes to what fungal infections really could do," Ferretti said. "It was scary, honestly. Some people went through so much before they actually got the treatment they needed. Even though I had an invasive fungal infection myself, I didn't really realize how bad it could be until I went to that conference. I guess I'm lucky because I got Dr. Spec on my team right away. He literally saved my life."
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 56% in the last seven years. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children's hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website






