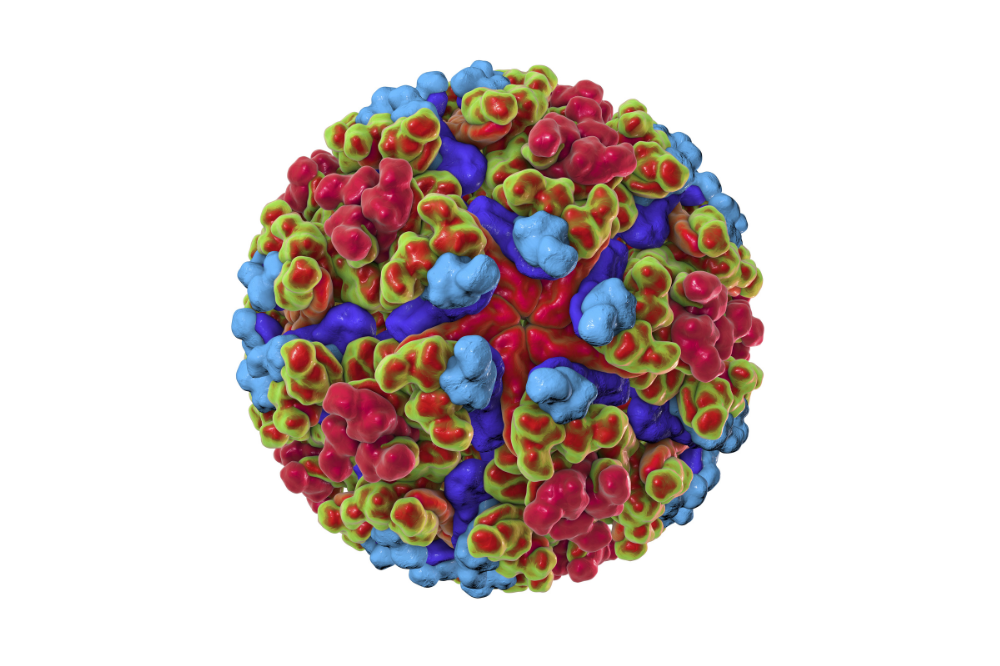
A 3D rendering of a chikungunya virus-like particle. (Credit: NIAID)
A new study published in PNAS suggests that rare cases of brain inflammation linked to live-attenuated yellow fever and Chikungunya vaccines were due to autoantibodies carried in a small subset of the population, most often older adults.
The FDA suspended the U.S. license for the live-attenuated chikungunya vaccine in August 2025 after adverse effects were reported; the only vaccine currently available in the U.S. cannot replicate or cause infection. In other parts of the world where the live virus vaccine is in use, the authors suggest that physicians screen potentially vulnerable individuals before vaccination, and steer those who test positive toward alternatives that do not rely on live viruses.
Chikungunya occurs in tropical and subtropical regions of Africa, the Americas, Asia, Europe, and islands in the Indian and Pacific Oceans. The virus spreads through the bite of a mosquito.
"We now know that a small percentage of people with these autoantibodies can end up with severe encephalitis if they receive this kind of Chikungunya vaccine," says Shen-Ying Zhang, associate professor of clinical investigation in Jean-Laurent Casanova's St. Giles Laboratory of Human Genetics of Infectious Diseases at Rockefeller. "So we strongly recommend screening people in countries still using this vaccine before administering it, especially if they are over age 65."
From Réunion to Rockefeller
The live-attenuated Chikungunya vaccine prevents disease by exposing the immune system to a weakened form of the virus, a mosquito-borne pathogen that causes fever and, in rare cases, life-threatening brain inflammation. It was released in 2023, but a handful of hospitalizations and deaths had been linked to the vaccine: two participants in a Phase III clinical trial involving thousands suffered serious reactions.
Concerns intensified in early 2025, during a mass vaccination campaign on the island of La Réunion, an overseas department of France in the Indian Ocean. In the United States, the Vaccine Adverse Event Reporting System issued an alert describing six serious adverse events, some involving brain inflammation, in people over age 65, while news reports in both the U.S. and France described deaths following vaccination.
To Zhang, these reports felt familiar. "When we read about these severe reactions in the news, we immediately suspected that it might be due to the autoantibodies that we study," she says.
This suspicion was grounded in more than a decade of research from Casanova's group. The lab has shown that a small subset of the population carries autoantibodies that neutralize type I interferons-molecules that normally serve as the immune system's earliest antiviral alarm. Live-attenuated vaccines rely on this antiviral alarm to keep weak viruses under control long enough for the body to develop immunity; the presence of these autoantibodies means that even an attenuated virus can potentially infect with impunity. In 2021, Casanova's lab published work implicating autoantibodies in one-third of life-threatening reactions to the live-attenuated yellow fever vaccine (about 10% of the adverse reactions reported were considered life-threatening), as well as in severe disease caused by regular viruses from COVID to West Nile.
Concerned that a similar pattern may be emerging with the Chikungunya vaccine, researchers from the Casanova lab reached out to colleagues overseas and offered to test whether the same immune defect observed in the yellow fever cases underpinned these events.
Screening for autoantibodies
To trace these rare reactions the team focused on five adults, ages 82 to 88, who developed serious complications after the vaccination campaign in La Réunion. They confirmed that the live vaccine virus was present in the bloodstream-and, in one severe case, the cerebrospinal fluid-of all five patients, showing that the virus had escaped the confines of the vaccine.
To understand why the immune system failed to contain an attenuated virus that should have been easy to control, the team tested blood and cerebrospinal fluid to see whether interferons could still activate frontline antiviral defenses. In several patients, the samples completely blocked interferon signaling, an effect that experiments ultimately traced to autoantibodies that neutralize type I interferons. Further, because the presence of these autoantibodies weeks after vaccination suggested that they were not a temporary response to the vaccine itself, but a permanent problem that had been silently weakening the immune system for some time.
Of the five patients tested, all three who developed brain inflammation carried high levels of autoantibodies, while the two with other severe outcomes did not, suggesting a link between this specific immune profile and encephalitis. Although based on a small number of cases, statistical analyses suggested a sharply elevated risk among individuals with these autoantibodies.
"This study suggests that severe disease due to the wild-type chikungunya virus, which is a rare outcome of infection, may be caused by the same autoantibodies," Casanova says.
Those carrying the antibodies were estimated to be more than 100 times more likely to experience a serious adverse event and more than 500 times more likely to develop vaccine-associated encephalitis. The risk, however, was not absolute. An estimated 1.2 percent of people ages 80 to 85 carry these high-risk antibodies, yet only a fraction of that population became ill, underscoring that the antibodies increase the risk of disease-but by no means guarantee it.
For those who become ill, the work points to a potential treatment option. The authors write that some patients may benefit from recombinant interferon-β therapy that could replace their frontline immune defenses. "As a first step, people who had severe reactions to the vaccine should have their autoantibodies tested and, if we know they carry this autoantibody, we can treat them patients with interferons that are not neutralized by the autoantibody," Zhang says.
But prevention may also be possible. In countries where the live virus vaccine is still available, the authors recommend screening older adults for these autoantibodies before administering it, and steering those who test positive toward safer options such as inactivated virus, recombinant protein, or mRNA vaccines.
In the meantime, much is still unknown. The present work is based on only five adverse cases; the authors therefore call for larger studies. "We need more epidemiological data to understand the global scope of severe reactions to this and other live vaccines," Zhang says. "These autoantibodies are not uncommon, and increase the risk of severe viral disease."






