Eating disorders are one of the deadliest forms of mental illness, but less than 20% of people with these disorders end up finding help.
"There's a huge need for access to care," said Ellen Fitzsimmons-Craft, an associate professor of psychological and brain sciences in Arts & Sciences and of psychiatry at the School of Medicine, all at Washington University in St. Louis.
There is limited access to mental health care providers in general, but even fewer trained therapists are available for eating disorders. Even if someone finds a clinic, there are often long waits and high treatment costs to pay, she added.
In response to this challenge, Fitzsimmons-Craft and colleagues, including Denise Wilfley, a professor of psychiatry at WashU Medicine, have been developing a range of digital cognitive-behavioral therapy-based interventions for eating disorders. Now, with a five-year $3.7 million grant from the National Institutes of Health (NIH) - and working with additional partners at the University of South Carolina and New York University - they will be optimizing a self-guided, chatbot-based digital intervention with the goal of making eating disorder counseling more readily available to all.
Previous research has shown that chatbots have the potential to help with behavior interventions, such as guiding people through smoking cessation counseling. But how these chatbots are designed matters immensely.
At this stage, those using ChatGPT-style large language models run the risk of polluting data with what the LLM pulls from the internet. A recent report found that these programs generated harmful content about eating disorders 41% of the time.
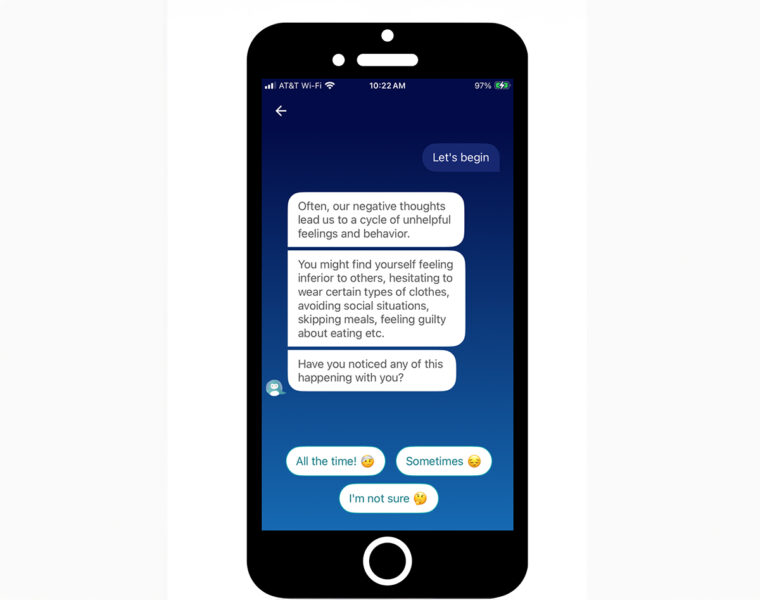
That will not be the case with this intervention, which is a rule-based artificial intelligence (AI) system, not generative AI at this stage, Fitzsimmons-Craft said. The current form of the chatbot is a closed system, carefully constructed with conversations written by experts in the field and optimized with user feedback. The tool will be hosted by Wysa, a global AI-led mental health company recognized for its best practices across clinical safety and privacy.
The scientists will test their approach with some 800 individuals with eating disorders who aren't currently in treatment. An "optimization randomized controlled trial" will help the researchers to understand which aspects of this self-guided cognitive-behavioral intervention work best. Ensuring the success of this intervention means determining which components are the most effective in reducing eating disorder symptoms, and, what order of components keep the user engaged, something that has not yet been tested in chatbots, Fitzsimmons-Craft said.
There are advantages to using chatbots for behavioral interventions, but the point is not to replace health-care providers.
"My goal has never been to replace people. I would love it if everyone could access a quality health-care provider, but that's not currently the case," Fitzsimmons-Craft said.
One main advantage is ease of entry. Because of shame associated with eating disorders, some people are not ready to talk to a real person about their challenges. "Even if they had access to care, they may not be willing or ready to do that," she said.
But it may be less scary to talk to an infinitely patient chatbot. For some people, it might be a far less intimidating first step to getting help. With further data from this project, Fitzsimmons-Craft and colleagues hope that eventually they can create personalized mental health interventions. From there, the tool will go to eating disorder and mental health nonprofits to share with the public.
"We have developed a lot of partnerships," she said. "I never want to do anything that's just going to sit around. I want to do science that can have a very near-term impact."






