In Alzheimer's disease, proteins like amyloid beta form clumps, known as plaques, that damage the brain.
But in some people, immune cells called microglia break down these proteins before they can cause harm. This leads to fewer and smaller clumps - and much milder symptoms.
Researchers at UC San Francisco identified a protein called ADGRG1 that enables microglia to gobble up and digest plaques. When the researchers removed this protein, which is a kind of receptor, from mice, their microglia barely nibbled on the plaques. This led to the rapid buildup of plaques, neurodegeneration and problems with learning and memory.
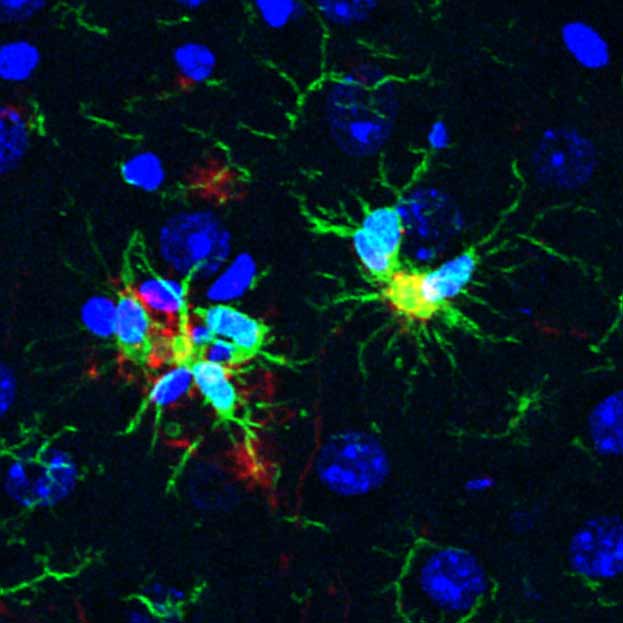
Normal microglia (green) are seen directly on top of amyloid beta plaques (red).
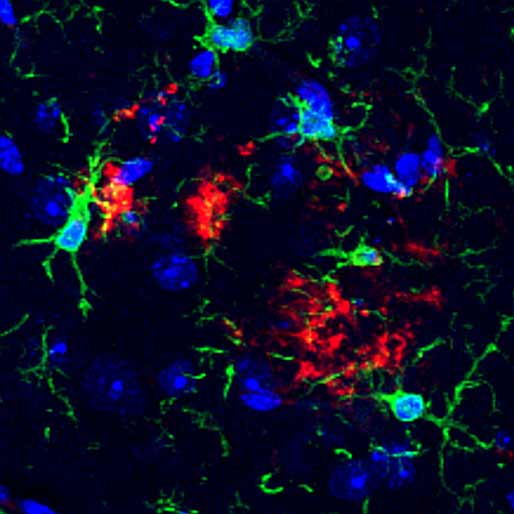
Microglia (green) lacking ADGRG1 receptor fail to find nearby amyloid beta (red).
"We think this receptor helps microglia do their job of keeping the brain healthy over many years," said Xianhua Piao , MD, PhD, a physician-scientist in the UCSF Department of Pediatrics.
Indeed, when the researchers reanalyzed a prior study of gene expression in the human brain, they found that individuals who died of mild Alzheimer's had microglia with lots of these receptors, and mild cognitive impairment - implying that the microglia ate well and kept the disease in check. But in those who died of severe Alzheimer's, the microglia had very few of the receptors, and the plaques proliferated.
ADGRG1 is part of a large family of receptors, called G protein-coupled receptors, that are routinely targeted in drug development. This bodes well for a rapid translation of the discovery into new therapies.
"Some people are lucky to have responsible microglia," Piao said. "But this discovery creates an opportunity to develop drugs to make microglia effective against amyloid-beta in everyone."
Paper: Neuron
Authors: Other UCSF authors are Beika Zhu, PhD, Andi Wangzhou, PhD, Diankun Yu, PhD, Tao Li, PhD, Rachael Schmidt, Stacy L. De Florencio, Lauren Chao, RN, Alicia L. Thurber, Minqi Zhou, Zeina Msheik, PhD, Yonatan Perez, PhD, Lea T. Grinberg, MD, PhD, Salvatore Spina, MD, PhD, Richard M. Ransohoff, MD, Arnold R. Kriegstein, MD, PhD, William W. Seeley, MD, and Tomasz Nowakowski, PhD.
Funding: This work was funded in part by the National Institutes of Health (P01AG019724, P50AG023501, R01NS094164, R01NS108446, K99AG081694), the Consortium for Frontotemporal Dementia Research, the Tau Consortium, the Alzheimer's Association (23AARG-NTF-1030341), the Cure Alzheimer's Fund, and the BrightFocus foundation postdoctoral fellowship (A2021020F).






