A research team led by the Department of Ophthalmology, School of Clinical Medicine, LKS Faculty of Medicine of The University of Hong Kong (HKUMed), with collaborators from the Faculty of Medicine of The Chinese University of Hong Kong (CU Medicine) and local and international partners, have developed a new technology ROTA (Retinal nerve fibre layer Optical Texture Analysis) to unveil the optical texture and trajectories of the axonal fibre bundles on the retina. ROTA outperforms the current clinical standards, attaining 15.0% to 28.4% higher in sensitivity in detecting early optic nerve damage in glaucoma – the leading cause of irreversible blindness. The research has been published in Nature Biomedical Engineering1 [link to publication].
Background
Glaucoma is the most common form of neurodegenerative disease. Whereas clinical diagnosis of glaucoma is predicated on the measurement of retinal nerve fibre layer (RNFL) thickness, typically obtained with a non-invasive digital imaging device, optical coherence tomography (OCT)2, false positives and false negatives are common, which renders clinical interpretation of OCT findings difficult, even for glaucoma specialists. This is supported by a meta-analysis reporting that the sensitivities of best-performing OCT parameters for detection of RNFL thickness abnormalities were only 65%-75% at specificities of 90%-95%3.
Research findings and significance
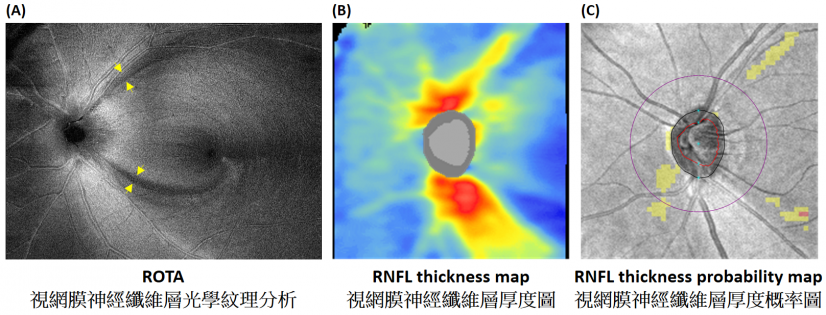
ROTA is a patented algorithm (US Patent No. 10,918,275)4 that integrates RNFL thickness and RNFL reflectance measurements obtained from standard OCT scans to discern the optical texture and trajectories of the axonal fibre bundles and reveal RNFL defects. ROTA can detect focal RNFL defects that are missed by standard clinical tests. Compared with OCT, ROTA can increase the sensitivity of detecting early optic nerve damage in glaucoma by 15-22%. At 95% specificity, the sensitivity of ROTA was 97.3-98.4% for detection of early glaucoma, 15.0% to 28.4% higher than the current clinical standards. HKUMed is working with the University of California San Diego (UCSD), the United States, to apply ROTA in research and patient care, while patients can find the application of ROTA at HKU Eye Centre and Southern District Hong Kong Eye Survey.
In a diagnostic study examining 177 healthy individuals and 363 glaucoma patients at the CUHK Eye Centre of CU Medicine, ROTA attained significantly higher sensitivity and specificity than conventional OCT RNFL thickness analysis to detect glaucoma1. Furthermore, ROTA is able to identify axonal fibre bundle damage in optic neuritis, ischemic optic neuropathy, and compressive optic neuropathy.
'We are delighted to have worked with CU Medicine to develop ROTA, which brings new hope to early identification and timely treatment of glaucoma due to its high sensitivity and specificity,' said Professor Christopher Leung Kai-shun, Chairperson and Clinical Professor of the Department of Ophthalmology, School of Clinical Medicine, HKUMed. 'Our next steps include enrolling patients from Queen Mary Hospital, Grantham Hospital, and Hong Kong Eye Hospital for longitudinal studies to examine the effectiveness of ROTA for detection of glaucoma progression, as well as working with OCT industrial partners to deploy ROTA in clinical care. Furthermore, HKU Eye Centre welcomes patients with questionable diagnosis of glaucoma for ROTA assessment.'
Professor Clement Tham Chee-yung, Chairman of the Department of Ophthalmology and Visual Sciences and S.H. Ho Professor of Ophthalmology and Visual Sciences, CU Medicine, remarked, 'Glaucoma can lead to irreversible loss of vision, if it is not diagnosed and treated early. In Hong Kong, about 25% of irreversible blindness is caused by glaucoma, and there are more about 100,000 glaucoma patients suffering from various levels of visual disability. Achieving earlier diagnosis of glaucoma and detection of progression through advanced imaging technologies is essential. I am glad that ROTA was developed by CU Medicine and HKUMed's collaboration and now it can be used in clinical practice.'
Clinical applications
ROTA underpins a highly sensitive and specific technique to advance the diagnosis of glaucoma and optic neuropathies. ROTA will be deployed on the Advanced Nerve and Glaucoma Imaging Network (ANGI Network), which comprises ophthalmologists, neuro-ophthalmologists and clinical researchers around the world. The committee members of ANGI Network include world-leading institutions in glaucoma research such as HKU, Asan Medical Center (Korea), Beyer Eye Institute at Stanford University (US), Moorfields Eye Hospital (UK), NTU Langone's Eye Center (US), and University College London (UK).
About the research team
This research was directed by Professor Christopher Leung Kai-shun, Chairperson and Clinical Professor of the Department of Ophthalmology, School of Clinical Medicine, as well as Director of HKU Eye Centre, HKUMed, the corresponding author of the study, and Dr Alexander Lam Ka-ngai, Research Officer of the Department of Ophthalmology, School of Clinical Medicine, HKUMed. Co-authors include Dr Carol Cheung Yim-lui, Associate Professor; Dr Kelvin Wan Ho-nam, Clinical Assistant Professor (Honorary); Dr Mandy Wong, Clinical Assistant Professor (Honorary); Dr Carmen Chan, Clinical Associate Professor (Honorary); Dr Noel Chan, Clinical Assistant Professor (Honorary); Dr Kam Ka-wai, Clinical Assistant Professor (Honorary) and Dr Lin Chen from the Department of Ophthalmology and Visual Sciences at CU Medicine; Professor Robert N. Weinreb, Chair and Distinguished Professor of the Department of Ophthalmology at UCSD; Professor Ted Garway-Heath, IGA Professor of Ophthalmology at the UCL Institute of Ophthalmology; Dr Marco Yu from Singapore Eye Research Institute; Philip Guo Yawen, Vivian Chiu and Gilda Lai from the Department of Ophthalmology, School of Clinical Medicine, HKUMed.
Acknowledgements
The research was supported by the General Research Fund (14101518), Hong Kong University Grants Committee and the Technology Start-up Support Scheme for Universities (2019-2020), Hong Kong Innovation and Technology Commission.