An international research team led by Professor Ian Wong Chi-kei, Head of the Department of Pharmacology and Pharmacy at LKS Faculty of Medicine of the University of Hong Kong (HKUMed) has just provided valuable evidence through a 20-year longitudinal study to address the longstanding debate concerning the potential impact of maternal diabetes on attention-deficit/hyperactivity disorder (ADHD) in children. This study, analysing real-world data from over 3.6 million mother-baby pairs in China's Hong Kong, Taiwan, New Zealand, Finland, Iceland, Norway and Sweden, showed that maternal diabetes during pregnancy is unlikely to be a direct cause of ADHD. The findings of this groundbreaking study were published today (8 April) in Nature Medicine [link to publication].
Background
Globally, approximately 16% of women have high blood sugar levels during pregnancy, and the prevalence of diabetes during pregnancy has been on the rise owing to factors like obesity and older maternal age. This can negatively affect the baby's brain and nervous system development. ADHD is one of the most common neurodevelopmental disorders in children, which can have severe negative consequences.1,2 Individuals with ADHD are prone to poor outcomes such as emotional problems, self-harm, substance misuse, educational underachievement, exclusion from school, difficulties in employment and relationships, and even criminality.3
The impact of maternal diabetes on the risk of ADHD in children has been a subject of debate because of inconsistent findings in previous studies. As a result, concerns regarding pregnancies in women with diabetes and the potential connection to the risk of ADHD in children have persisted. Recognising the importance of identifying risk factors for ADHD, especially for women of childbearing age, the cross-regional study, funded by the Hong Kong Research Grants Council, utilised population-based data from China's Hong Kong, Taiwan, New Zealand, Finland, Iceland, Norway and Sweden to comprehensively assess the association between maternal diabetes and the risk of ADHD in offspring.
Research methods and findings
This extensive study, which included a remarkable sample size of over 3.6 million mother-child pairs from 2001 to 2014, with follow-up until 2020, yielded crucial observations regarding the association between maternal diabetes during pregnancy and the risk of ADHD. The research team first found that children born to mothers with any type of diabetes, whether before or during pregnancy, had a slightly higher risk of ADHD compared to unexposed children, with a hazard ratio of 1.16. The study further identified elevated risks of ADHD for both gestational diabetes (diabetes during pregnancy) and pregestational diabetes (diabetes before pregnancy). The hazard ratio for gestational diabetes was 1.10, indicating a modestly increased risk, whereas the hazard ratio for pregestational diabetes was 1.39, suggesting a more substantial association.
However, an intriguing finding emerged when the research team compared the risk of ADHD between siblings with discordant exposure to gestational diabetes and found no significant difference. This unexpected result indicates that the previously identified risk of ADHD when children were exposed to gestational diabetes during pregnancy is likely due to shared genetic and familial factors, rather than gestational diabetes per se. These findings challenge previous studies that suggested maternal diabetes during or before pregnancy could heighten the risk of ADHD in children.
Research significance
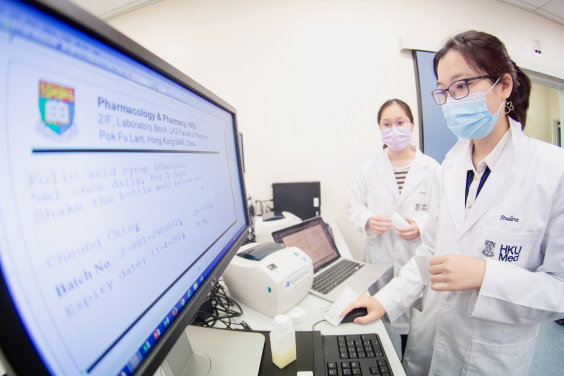
According to Professor Ian Wong Chi-kei, Lo Shiu Kwan Kan Po Ling Professor in Pharmacy, and Head of the Department of Pharmacology and Pharmacy, HKUMed, the process of coordinating with renowned scholars from around the world analysing cross-regional cases spanning over 20 years was no mean feat. This collaborative effort aimed to establish a comprehensive understanding of the matter at hand.
'In contrast to previous studies, which hypothesised that maternal diabetes during pregnancy could significantly increase the risk of ADHD, our study found only a modest association between maternal diabetes and ADHD in children after considering the intricate interplay of various influential factors. Notably, sibling comparisons showed this association is likely influenced by shared genetic and familial factors, particularly in the case of gestational diabetes,' explained Professor Wong.
He highlighted the need for deliberate consideration and future research. 'This implies that women who are planning pregnancy should look at their holistic risk profile rather than focusing solely on gestational diabetes,' he said. 'Moving forward, it is crucial for future research to investigate the specific roles of genetic factors and proper blood sugar control during different stages of embryonic brain development in humans.
About the research team
The research was jointly led by Professor Ian Wong Chi-kei, Lo Shiu Kwan Kan Po Ling Professor in Pharmacy, and Head of the Department of Pharmacology and Pharmacy, HKUMed; Dr Kenneth Man Keng-cheung, Honorary Assistant Professor of the Department of Pharmacology and Pharmacy, HKUMed, and Lecturer of the School of Pharmacy, University College London; Dr Carolyn Cesta, Assistant Professor of the Centre for Pharmacoepidemiology, Karolinska Institute, Sweden; Professor Edward Lai Chia-cheng, School of Pharmacy, National Cheng Kung University, Taiwan; Professor Helga Zoega, Associate Professor of the School of Population Health, Faculty of Medicine and Health, UNSW Sydney, Australia. The first authors were Dr Adrienne Chan Yu-ling, Senior Research Assistant, and Dr Gao Le, Postdoctoral Fellow, Department of Pharmacology and Pharmacy, HKUMed; Dr Miyuki Hsieh Hsing-chun, School of Pharmacy, National Cheng Kung University, Taiwan; and Dr Lars Kjerpeseth, Department of Chronic Diseases, Norwegian Institute of Public Health.
Other members in the research team included experts in child psychiatry and epidemiology. They were Dr Raquel Avelar; Professor Tobias Banaschewski; Dr Amy Chan Hai-yan; Professor David Coghill; Dr Jacqueline M Cohen; Dr Mika Gissler; Professor Jeff Harrison; Professor Patrick Ip Pak-keung, Clinical Professor, Department of Paediatrics and Adolescent Medicine, School of Clinical Medicine, HKUMed; Dr Øystein Karlstad; Dr Wallis CY Lau, Honorary Research Associate, Department of Pharmacology and Pharmacy, HKUMed; Dr Maarit K Leinonen; Dr Leung Wing-cheong; Liao Tzu-chi; Dr Johan Reutfors; Dr Shao Shih-chieh; Professor Emily Simonoff; Professor Kathryn Tan Choon-beng, Department of Medicine, School of Clinical Medicine, HKUMed; Professor Katja Taxis; and Andrew Tomlin.
Acknowledgements
This work was supported by the General Research Fund of the Hong Kong Research Grants Council.