A scientific instrument at the Department of Energy's Oak Ridge National Laboratory could help create a noninvasive cancer treatment derived from a common tropical plant.
Pancratistatin is a chemical compound found in the spider lily, a native Hawaiian flower. Unlike traditional treatments, it kills cancer cells while keeping healthy cells intact.
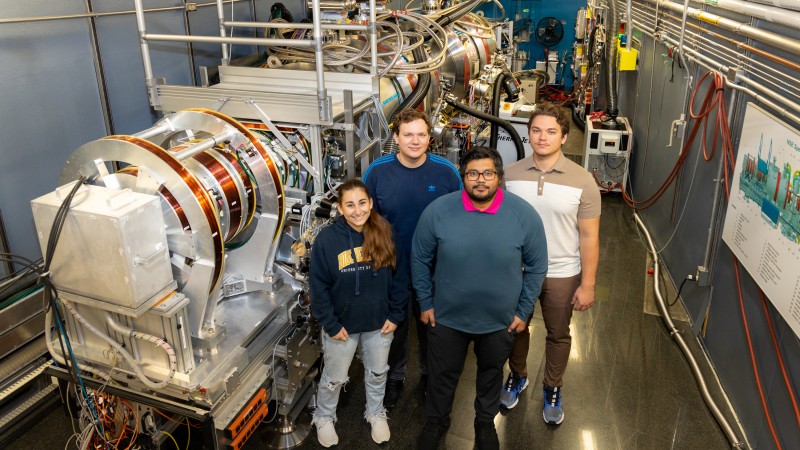
Until recently, pancratistatin's workings have mystified scientists, clouding hope for potential new treatments. But after conducting neutron experiments at ORNL, students from the University of Windsor have gained fundamental insights into the mechanics of pancratistatin that could open new doors to much-improved cancer treatments.
"By experimenting with cellular extracts here at the lab, we're building on previous work to get a more detailed picture for pancratistatin," said Stuart Castillo, the UWindsor doctoral candidate leading the study. "Our hope is to create a new path for treating cancer that doesn't damage healthy cells."
ORNL's Spallation Neutron Source provides one of only a handful of neutron beamlines in the world capable of making the kinds of measurements the study needed. The Neutron Spin Echo instrument allowed the students to simultaneously measure cellular dynamics in angstroms and microseconds. One angstrom equals one ten-billionth of a meter. One microsecond equals one millionth of a second.
Cancerous tumors begin with an overgrowth of cells, a process that starts in mitochondria, the parts of a cell that produce energy. In theory, cancer cells get an influx of cholesterol that stiffens mitochondria's cellular walls, or membranes, stopping their communication with other parts of the cell. Then, the mitochondria go rogue, causing cells to overmultiply.
One step back, one leap forward
Decades ago, scientists used living cells to discover pancratistatin's effect on cancer. In these early experiments, pancratistatin successfully triggered apoptosis, or cell death, in cancerous testicular, breast, liver, pancreatic and nerve cells. Since then, research has been confined to experiments on synthetic membranes until more could be understood about this natural remedy. Experimenting with synthetic material allows researchers to build their understanding of specific changes without the variables that come with living systems.
"Something we say about working with synthetic membranes is that it's never 100% representative of a cell and never will be. The scientific community as a whole eventually wants to transition from this basic synthetic model to a more realistic cell model," said UWindsor graduate researcher Maksymilian Dziura. "We want to use living cells to understand cells, but getting there isn't easy. We need to fully understand the picture before we can slowly transition into using more realistic systems."
SNS and its sister facility, the High Flux Isotope Reactor, provide essential tools to help researchers observe and measure materials at the atomic scale. Neutrons are particularly suited for investigating biological membranes, because neutrons can pass through delicate biological materials without damaging them. Before coming to ORNL, the students showed that pancratistatin stiffened synthetic mitochondrial membranes in a way that triggered apoptosis, providing the basis for working with cells.
The students used SNS's Neutron Spin Echo spectrometer to compare how pancratistatin affects the inner and outer layers of the mitochondria's membranes in cancerous and noncancerous cells.
"We're looking specifically at how stiff the membrane is, how thick it is and how those molecules behave next to each other," said UWindsor graduate researcher Dominik Dziura. "The thought is that a healthy membrane will be flexible and move like it's supposed to, binding to other receptors and membranes and allowing communication between cells, unlike the cancerous membranes."
"There's so much we don't know about cancer," said UWindsor graduate researcher Isabelle Dib. "And we haven't really looked at the differences between cancerous and noncancerous cellular membranes. This is a new approach."
The team also used labs at the ORNL's Shull Wollan Center Center for Nanophase Materials Sciences to develop and prepare their samples. Both are a short walk to SNS. The proximity of these resources enabled the team to do research a few short weeks that otherwise could have taken them months or longer.
"The setup we have here, with SNS, the Shull Wollan Center and CNMS, it's perfect for us to conduct our experiments and analyze our data," said Castillo. "It's the whole package."
This research was supported by the University of Tennessee Shull Wollan Center, co-located at ORNL.






