Exposure to the virus that causes COVID-19 may lead to chronic health impacts that, in some cases, may become apparent only years later, according to new research in nonhuman primates led by Oregon Health & Science University.
The study, published today in the journal PLOS Pathogens, raises the possibility that long-COVID may be far more common than currently estimated.
More articles and photos in a media kit about the Oregon National Primate Research Center.
Long COVID is generally defined as a chronic illness with a range of symptoms or conditions that can last weeks, months or even years after the initial illness. Its prevalence can be hard to determine because the symptoms are largely self-reported, but researchers have reported it affects as many as one in 10 people.
The new close examination of infected nonhuman primates suggests that figure may be much higher.
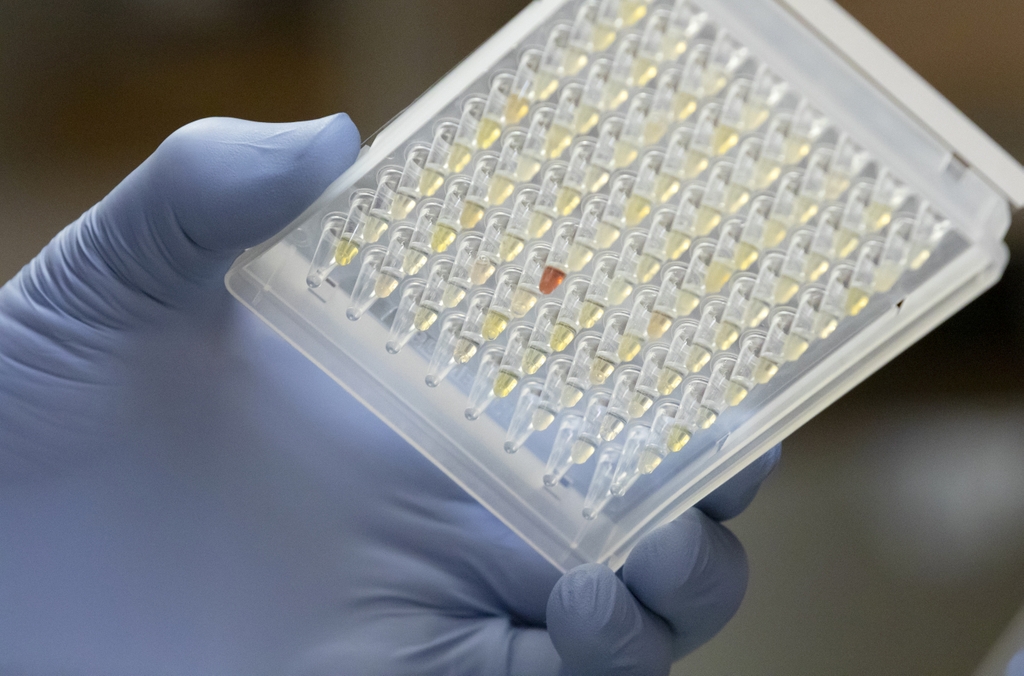
Researchers examined both tissues and blood biomarkers in a group of rhesus macaques exposed to the delta variant of the SARS-CoV-2 virus, which emerged relatively early in the pandemic at a point when many people had yet to be vaccinated or naturally exposed. Researchers monitored the macaques over six months and found persistent parameters of disease in 60% to 90% of the animals, even though the overt symptoms appeared relatively mild.
Researchers say the findings may be validating for many people.

"It may give affirmation to a lot of people who experience lingering symptoms that are being dismissed or they try to ignore," said lead author Kristin Sauter, Ph.D., research assistant professor at OHSU's Oregon National Primate Research Center. "This may provide proof that long COVID is affecting a lot more people than we think."
Researchers found evidence for lung pathology, sleep disturbance and changes in blood biomarkers that predict the risk for cardiometabolic conditions such as hypertension, obesity and insulin resistance. The animals were studied for six months, but these findings suggest the potential for diseases to develop months or years after the initial infection.
They say the findings should raise awareness among clinicians and patients alike.
In the next stage of research, the team intends to test early interventions in nonhuman primates, an area of research that could be especially relevant for people with underlying metabolic conditions such as obesity or even prediabetes.

"We're proposing a study to see if we can mitigate some of the metabolic changes we see following infection," said senior author Charles Roberts, Ph.D., professor and senior adviser at the Oregon National Primate Research Center. "We intend to look at potential interventions to institute at the time of infection for at-risk populations."
Scientists generally recognize COVID-19 has more severe effects on people with underlying medical conditions. Conversely, the new research set out to examine why a SARS-CoV-2 infection may put people at higher risk of developing obesity and diabetes.
The study compared the effects of SARS-CoV-2 in two groups of macaques, nine that were overweight and 10 that were lean and metabolically healthy. Researchers found different long-term consequences in each group; however, the lean animals did not avoid health impacts from exposure to the delta variant.
"Even if you started off lean and healthy, this study shows it won't protect you from some of the worst consequences of COVID," Roberts said.
This research was supported by the National Institutes of Health's National Institute of Diabetes and Digestive and Kidney Diseases award 3R01DK122843, as part of the NIH's Researching COVID to Enhance Recovery, or RECOVER Initiative, which seeks to understand the long-term effects of COVID and improve long COVID care. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
All research involving animal subjects at OHSU must be reviewed and approved by the university's Institutional Animal Care and Use Committee (IACUC). The IACUC's priority is to ensure the health and safety of animal research subjects. The IACUC also reviews procedures to ensure the health and safety of the people who work with the animals. The IACUC conducts a rigorous review of all animal research proposals to ensure they demonstrate scientific value and justify the use of live animals.






