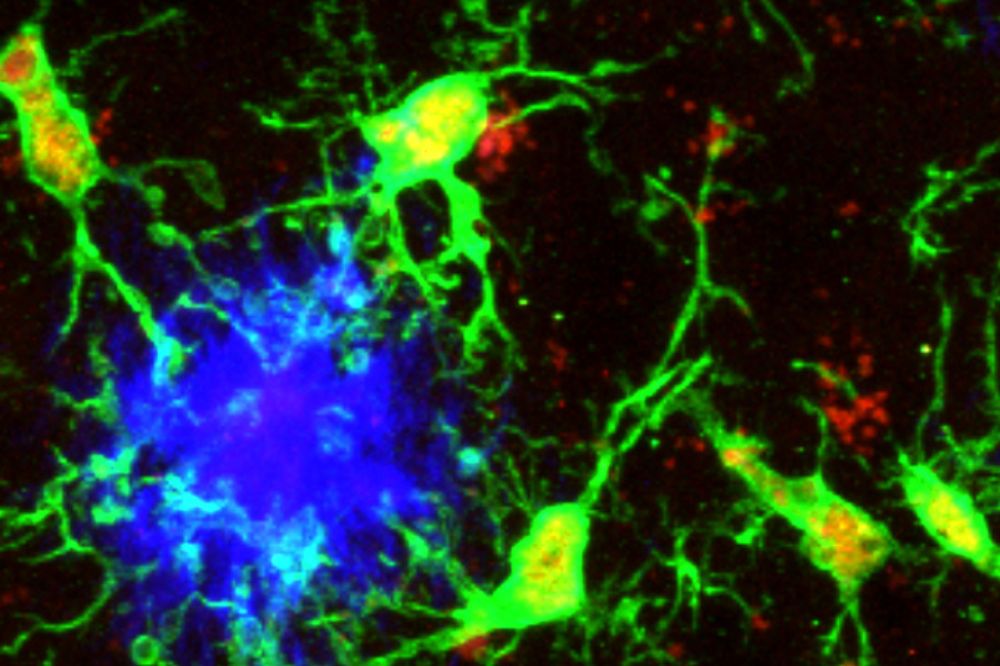
Microglia (green) responding to aggregated beta-amyloid plaques (blue) in the mouse cortex. (Credit: Jessica M. Crowley)
A previously unknown population of immune cells in the brain may act as natural defenders against Alzheimer's disease, according to a new study in Nature.
The researchers found that a subset of microglia-the brain's resident immune cells-can shift into an anti-inflammatory state that shields neurons from damage, revealing unexpected parallels between the brain's immune system and B and T cells that protect the rest of the body. In collaboration with scientists from the Max Planck Institute, the Icahn School of Medicine at Mount Sinai, The City University of New York, and other international partners, Rockefeller researchers showed that enhancing this protective state in mouse models quieted brain inflammation, slowed the spread of toxic tau, and reduced amyloid plaque buildup. The findings reveal a molecular pathway that may explain differences in Alzheimer's susceptibility and suggest new ways to harness the brain's own immune system to combat neurodegeneration.
"It is remarkable to see that molecules long known to immunologists for their roles in B and T lymphocytes also regulate microglial activity," says Alexander Tarakhovsky, head of the Laboratory of Immune Cell Epigenetics and Signaling at Rockefeller. "This discovery comes at a time when regulatory T cells have achieved major recognition as master regulators of immunity, highlighting a shared logic of immune regulation across cell types. It also paves the way for immunotherapeutic strategies for Alzheimer's disease."
Flipping the switch
Microglia play a pivotal role in Alzheimer's disease-both as protectors and aggressors. Depending on gene expression, the brain's own immune cells have at times been shown to clear toxic amyloid deposits and, at other times, to drive chronic inflammation. The question was which precise molecular cues determined whether microglia would play a helpful or harmful role.
Prior work had hinted that the transcription factor PU.1 was likely one piece of the puzzle. Genetic analyses revealed that a common mutation in the gene encoding PU.1 reduces its expression in myeloid cells, a lineage that includes microglia, and that people carrying this mutation tend to develop Alzheimer's later and experience milder symptoms. Earlier work also showed that PU.1 regulates Alzheimer's-related genes in human microglia and that modest shifts in its activity can alter how these cells respond to inflammation. But the specific molecular pathway or mechanism linking PU.1, microglia, and Alzheimer's progression, remained elusive.
To address these questions, the team combined molecular profiling, genetic manipulation in mice, and analysis of human brain tissue to map the PU.1 pathway. Imaging revealed a small group of microglia with low levels of the transcription factor PU.1 clustering around amyloid plaques in both mice and humans. These immune cells proved unusually resilient-a drug that usually destroys microglia had little impact on this population. Examining the survivors revealed that microglia low on PU.1-low activated CD28 along with a suite of molecules known for calming inflammation elsewhere in the body. The results suggested that these microglia had entered a protective state to stabilize the brain's environment and limit further damage.
Subsequent experiments revealed how this protective shift in microglia is triggered. When plaque-sensing receptors on microglia-such as TREM2 and CLEC7A, which detect debris and abnormal proteins-were activated, they launched a signaling cascade through two key molecules, SYK and PLCγ2, which in turn lowered PU.1 levels and activate the microglia's protective mode. Further, the team found that simply reducing PU.1 was enough to turn on CD28 and other anti-inflammatory genes in mice, while increasing PU.1 made microglia more inflammatory.
In mice genetically engineered to display symptoms of Alzheimer's, the effect was striking-the low-PU.1 state shut down harmful immune pathways that normally release toxic molecules, reduced the hallmarks of cellular stress in microglia, compacted amyloid plaques into less damaging forms, prevented the spread of the tau protein that kills neurons, and ultimately preserved memory and extended lifespan. But when the CD28 gene was deleted in these mice the protective effects were lost. Inflammation returned, amyloid plaques expanded, and the disease progressed more rapidly, despite the low-PU.1 state of the microglia.
Together, the results revealed a PU.1-CD28 axis in which signals from plaque-sensing receptors activate a pathway that lowers PU.1 levels and switches on CD28, pushing microglia into a neuroprotective state that suppresses inflammation, limits amyloid and tau buildup, preserves brain function and lifespan, and relies entirely on CD28 to maintain these effects.
"This finding extends our earlier observations on the remarkable plasticity of microglia states and their important roles in diverse brain functions," says Anne Schaefer, senior author and a former Rockefeller postdoc in the Greengard laboratory who is now a directs the Max Planck Institute for Biology of Ageing.
Rethinking the brain's immune system
In the broadest sense, the findings reshape our understanding of immunity in the brain itself, revealing that the same molecular logic guiding the body's general immune system may also be at work in the central nervous system. Molecules such as CD28, once thought exclusive to T and B lymphocytes, were shown to regulate microglial activity, a discovery that underscores surprising parallels between how suppressor T cells prevent autoimmunity and how PU.1-low, CD28-positive microglia limit neuroinflammation in the brain. Together, these insights suggest that the brain's immune system is not an isolated entity but part of a broader, evolutionarily conserved network of checks and balances designed to preserve tissue health.
The discovery of the PU.1-CD28 axis in microglia also offers a blueprint for how the brain's immune system protects itself from Alzheimer's. By uncovering an internal circuit of immune regulation that can be steered toward protection rather than inflammation, the work points to the possibility of therapies that train the brain's own defenses to fight neurodegeneration. Future efforts to understand how PU.1-low, CD28-positive microglia interact with neighboring cells could pave the way for a new generation of immune-based strategies to preserve brain health.






