When a car accident or athletic injury destroys more than 20% of a muscle's mass, the body faces a problem it often can't heal fully on its own. Without intervention, scar tissue fills the injury site and can leave patients with permanent weakness and limited mobility.
Now, researchers at the University of Oregon's Knight Campus, led by Alycia Galindo, a PhD candidate in Marian Hettiaratchi's lab, are developing a potential solution: microscopic scaffolds that guide muscle cells to regenerate organized, functional tissue. Their findings, published in the September edition of Cellular and Molecular Bioegineering, and part of the 2025 Young Innovator collection, combine microstructures with biochemical cues, offering a blueprint for future medical technologies that could help damaged muscle heal faster and more effectively.
Coaxing muscle to regenerate isn't straightforward. Muscles are intricate structures built from thousands of precisely organized fiber bundles, composed of different proteins like actin and myosin, that must work together to contract and move.
Current approaches, like muscle transplants, often fail because they struggle to integrate into the structure of existing muscle, often resulting lots of scar tissue and in impaired function.

Bioengineering PhD candidate Alycia Galindo, a student in Marian Hettiaratchi's lab, wanted to overcome this challenge by providing regenerating muscle cells with microscopic scaffolds they could follow as they regenerate. The idea is that these tiny scaffolds could provide a roadmap for these cells to follow as they regenerate and eventually form the complex structure of mature muscle and, hopefully, enable more functional recoveries.
Galindo first teamed up with Kelly O'Neill, another graduate student in the Knight Campus, who is supervised by Paul Dalton, an associate professor in bioengineering and the Bradshaw and Holzapfel Research Professor in Transformational Science and Mathematics. This initial partnership grew out of the Wu Tsai Human Performance Alliance, an effort that brings together researchers focused on understanding peak performance and advancing human health.
Dalton is the inventor of a technology called melt electrowriting (MEW), a micro 3D printing technique that enables the production of microscopic scaffolds with precise geometries. The technique works by melting biocompatible polymers and using electrical forces to draw them into tiny fibers-just micrometers wide-stacking them layer by layer into three-dimensional structures.
"What makes MEW special is the level of control we have," Dalton explains. "It's really cool to think about applying it with muscle cells in this way."
Galindo started by attempting to grow developing muscle cells, called myoblasts, on MEW structures, which look like tiny grids (see left picture). She tested different scaffold thicknesses, ranging from 10 to 30 micrometers (about 1/10th the width of a human hair), and found that the myoblasts grew best on the 20-micrometer structures. This size likely worked best because it closely matches the diameter of muscle cells. While some cells attached and grew on the MEW scaffolds, there was still room for improvement.
"We thought that combining MEW structural scaffolds with biochemical signals could be really powerful," says Marian Hettiaratchi, an associate professor of bioengineering and senior author on the paper. "Cells respond to both physical and chemical cues in their environment. Giving them the combination of physical and chemical cues could really help the muscle cells."
Galindo then coated the MEW scaffolds with hyaluronic acid-a molecule familiar from skincare products that also occurs naturally in the body-because it mimics the cellular microenvironment and helps cells adhere and grow. Compared to scaffolds with no hyaluronic acid coating, they found that the hyaluronic acid increased the surface area available for cell attachment and resulted in more myoblasts growing on the scaffolds.
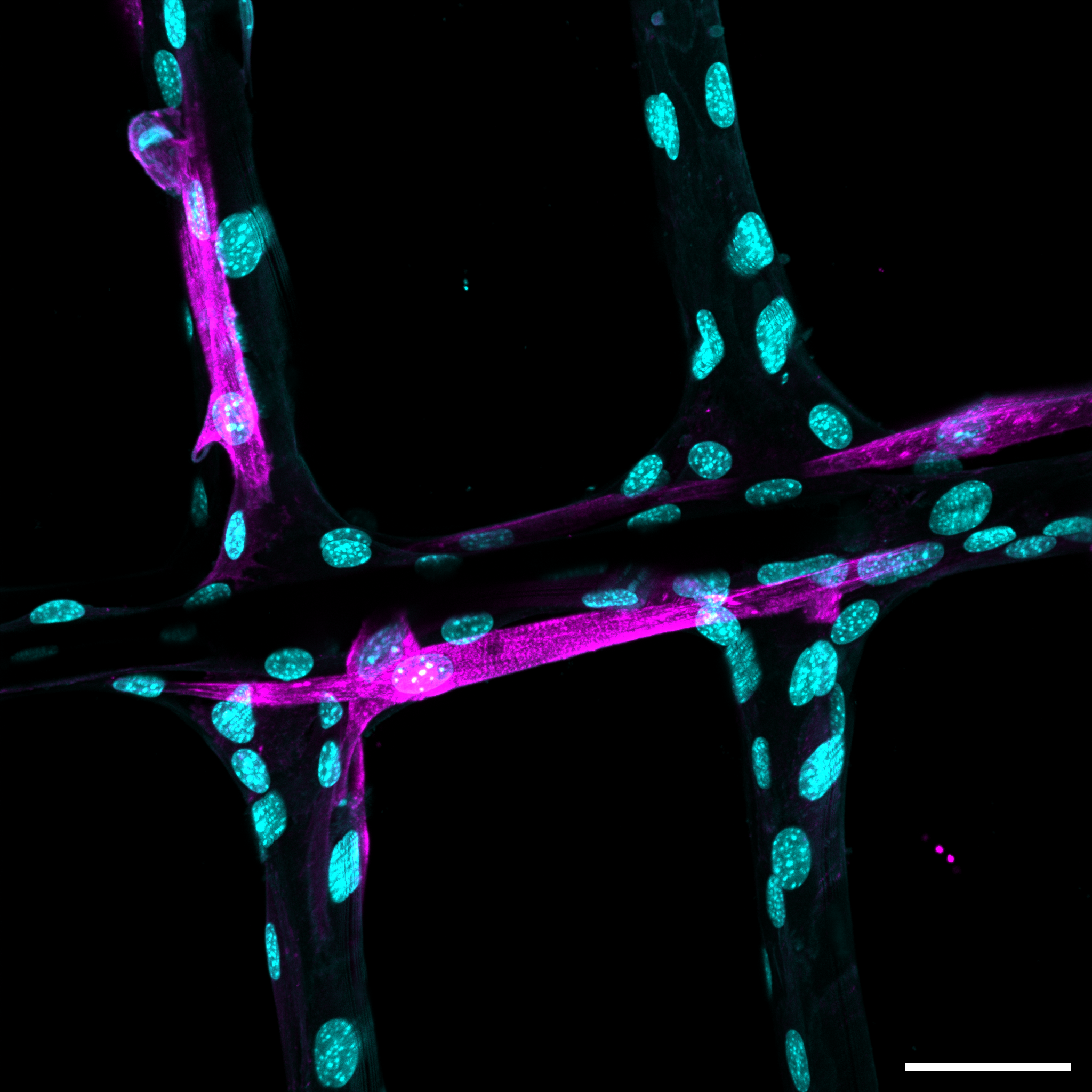
Finally, Galindo wanted to use another common approach from the Hettiaratchi lab: the use of cell instructive molecules. These are molecules that trigger different responses from cells, like directing them to grow or attach. Previous work in the Hettiaratchi lab has focused on delivering these molecules to optimize regeneration after injuries. Galdino added a molecule that promotes cellular attachment, a peptide called RGD, to the scaffolds. When she added RGD to the hyaluronic acid coating, the myoblasts stuck to the scaffolds significantly better than the uncoated scaffold versions.
Not only did the myoblast cells stick to these RGD coated scaffolds better , they began to align into structures that mimic muscle organization, and also began to differentiate into mature muscle cells.
"The difference was really dramatic," Galindo recalls. "With RGD, the cells not only attached more readily, but they also wrapped around the fibers and began growing along them in an organized fashion. These cells were using the scaffold as a template for regeneration."
While this technology remains a long way from human use, it represents a significant step toward developing effective therapies for large muscle injuries. This approach, combining structural scaffolds with customizable biochemical signals, could potentially be adapted for different types of injuries or patient needs.
"We've shown proof of concept with one set of molecules and one scaffold design. Now we can start optimizing-testing different growth factors, different release patterns, and different architectural arrangements. There's a huge design space to explore" says Hettiaratchi.
The team envisions future versions of the technology that could be implanted during surgery or even injected as a gel that solidifies into a scaffold at the injury site. The scaffold would provide both structural support and time-released biochemical signals, gradually degrading as the muscle regenerates until only healthy, functional tissue remains.
"We're not there yet," Galindo cautions, "but we've demonstrated that you can engineer scaffolds at the microscale that muscle cells recognize and respond to. That's a critical first step toward building therapies that can truly restore function after severe muscle loss."
The research was supported by the Wu Tsai Human Performance Alliance, the National Institutes of Health, and the Bradshaw and Holzapfel Research Professor in Transformational Science and Mathematics.






