Lactate, thought to by a byproduct of cell respiration, plays a central role in the potentially lethal immune reaction
The World Health Organization estimates that around six million people worldwide may die of sepsis every year, and the CDC reports that one in three patients who die in the hospital have sepsis. Sepsis, sometimes called septic shock, is caused by the immune system overreacting to an infection and causing damage to vital organs; it has been implicated recently in deaths from COVID-19. A team at the Weizmann Institute of Science has uncovered a molecular mechanism that plays a central role in the dangerous spiral of sepsis, and their findings suggest a way of reining in the immune system and preventing lethal organ damage.
The first immune cells out of the gate at the onset of an infection are white blood cells known as neutrophils. Neutrophils are born in the bone marrow, released into the blood stream, and they return to the bone marrow to die. Fierce warriors, neutrophil have a dark side: They can get out of hand and rampage through the body, mercilessly damaging living tissue. A standard blood test for sepsis looks at levels of neutrophils as well as checking for a substance called lactate, which is known to be produced at higher than average levels in sepsis. Lactate is produced in the process of cell respiration, and it was thought to be a byproduct of these cells - one the body simply removed once it was secreted. Dr. Eman Khatib-Massalha, a postdoctoral fellow in the group of Prof. Tsvee Lapidot of the Institute's Immunology Department, thought there might be a deeper connection between neutrophils and lactate and she decided to investigate.
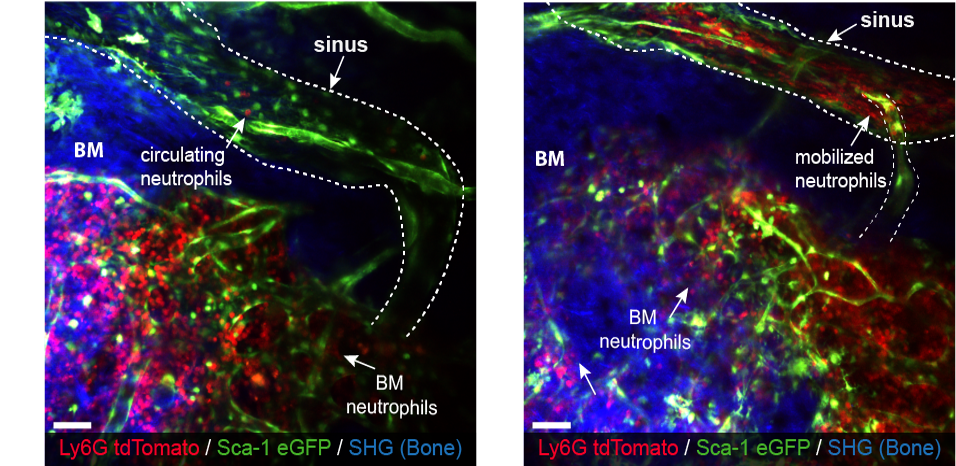
The research team included Staff Scientist Dr. Orit Kollet and other members of Lapidot's lab, Ph.D. student Adi Biram in the group of Dr. Ziv Shulman of the Immunology Department and postdoctoral fellow Dr. Hassan Massalha in the lab of Prof. Shalev Itzkovitz of the Molecular Cell Biology Department. Their first observation was that neutrophils seem to specialize in lactate production and secretion early in the process of fighting infection. Working with mouse models of infection, they found that there was a rise in free radicals by the bone marrow (BM) neutrophils, as well as in a transcription factor called HIF1-alpha, which was known to be active in the cells' response to conditions of low oxygen. Increases in these two then led to an increase in levels of an enzyme that produces lactate in cells. This is how the reaction to infection led to a rise in lactate levels. Not only did the cells produce more lactate, there was a corresponding rise in lactate transport in the cell membrane for secreting the metabolite outside the cell.
If we could block lactate secretion, we might stop neutrophil levels from rising too much and thus we could prevent sepsis
Did this extra lactate serve a purpose? The researchers genetically engineered mice to interfere with the lactate production chain - either preventing the production of free radicals or silencing the HIF1-alpha transcription factor. In both cases, lactate production dropped, but the researchers were surprised to find that the net effect of blocking lactate was to stop the neutrophils from leaving the bone marrow for the bloodstream. When these engineered mice had their lactate levels restored, the neutrophils once again flocked out of the bone marrow.
To find the exact mechanism by which the neutrophils exit the bone marrow following lactate treatment, the researchers followed the lactate trail, uncovering another chain of events. To get into the bloodstream, neutrophils must get past the tight seals of the BM blood vessels. The lactate latches on to endothelial cells in the bone marrow; for the first time, the researchers identified a special lactate receptor on these cells, called GPR81. This then causes the levels of another protein - VE-Caderin - to drop, which then lets spaces large enough for the neutrophils to slip through to open up in the blood vessels running through the bone marrow.
To confirm these findings, the scientists gave lactate to mice engineered to lack that particular receptor. Despite high levels of lactate, the neutrophils mostly remained in the bone marrow, although the researchers were surprised to find that their levels dropped by around 60%, some clearly still finding their way into the bloodstream by other means. Continuing to investigate, they found evidence that lactate is not only more than a mere byproduct, it plays a central role in sepsis, causing the production of cytokines and chemokines - both contributors to the damage inflicted by out-of-control immune reactions.
"The findings suggest that if we could block lactate secretion, we might stop neutrophil levels from rising too much and thus we could prevent sepsis," says Khatib-Massalha. "There are already some substances that could reduce lactate levels; these are in the approval process for other medical conditions. Some day they might be used to treat acute inflammation, especially sepsis."
The researchers took the first step in demonstrating how such a drug would work, injecting lactate inhibitors into mouse models of inflammation. In these mice, neutrophil levels dropped and the dangerous inflammation dropped to safe levels.
Also participating in this research were Prof. Ronen Alon of the Institute's immunology Department and Dr. Amiram Ariel of Haifa University.
Lactate in the bone marrow introduces neutrophils (red) into circulation. Green are blood vessels and endothelial cells
On her way to Cambridge
A few days after the study's results were published, Dr. Eman Khatib-Massalha learned she would be the recipient of the dean's prize for excellence, as well as receiving an award to help women postdoctoral fellows continue their research abroad. In addition, she was chosen valedictorian for the Feinberg Graduate School graduation ceremony.
That award, in addition to other grant will help Khatib-Massalha, her husband Dr. Hassan Massalha and their two-year old daughter go to Cambridge University, where she will continue to research the immune system.
Eman met Hassan when she was an MSc student at Haifa University and he was getting his PhD in the group of Prof. Asaph Aharoni in the Institute's Plant and Environmental Sciences Department. At first, she recalls, she resisted Hassan's suggestion she apply to the Weizmann Institute of Science, preferring to stay in her MSc track in Haifa. But once she came to visit, "I already knew, in that first visit, that as a researcher this was the right place for me," she says.
"Hassan finished his doctorate three years ago. While he waited for me to finish mine, he completed a stint of postdoctoral research in Prof. Shalev Itzkovitz's lab and became an expert in genetic sequencing, Now, by going abroad together, we have a chance to start over, together," she adds.
Prof. Tsvee Lapidot's research is supported by the Steven B. Rubenstein Research Fund for Leukemia and Other Blood Disorders; the Dr. Beth Rom-Rymer Stem Cell Research Fund; the Henri Gutwirth Fund for Research; the Hadar Impact Fund; and Asher Pertman and Wayne Pertman. Prof. Lapidot is the incumbent of the Edith Arnoff Stein Professorial Chair in Stem Cell Research.






