Two epidemiology studies led by researchers of the University of Hawaiʻi Cancer Center have been selected as research highlights of the National Cancer Institute's Epidemiology and Genomics Research Program (EGRP). The publications were among 36 selected studies that were funded by EGRP in 2020. Both studies used data from the UH Cancer Center's Multiethnic Cohort (MEC) Study, a large epidemiological study that follows residents of Hawaiʻi and Los Angeles for the development of cancer and other chronic diseases.
- Related UH News story: Cancer, diabetes findings unlocked by world's most ethnically diverse study, March 7, 2021
This research is an example of UH Mānoa's goal of Excellence in Research: Advancing the Research and Creative Work Enterprise (PDF), one of four goals identified in the 2015-25 Strategic Plan (PDF), updated in December 2020.
Cancer risk, intra-abdominal fat
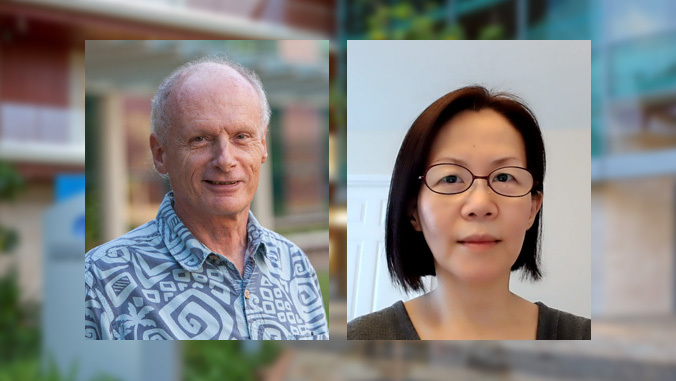
In one publication led by Loïc Le Marchand, researchers demonstrated that intra-abdominal fat, also known as visceral adipose tissue (VAT), could be predicted using common biochemical markers in blood, and that the predicted VAT was associated with cancer risk. They found that women with a high VAT score in the MEC Study were at greater risk for developing breast cancer, even at comparable levels of body weight or total body fat.
VAT is known to have more harmful metabolic effects than the fat found underneath the skin. Investigators had reported earlier that VAT amounts vary substantially by race/ethnicity at a given body weight, which may explain obesity-related cancer disparities. "Since accurate VAT measurement requires expensive imaging tests, the assessment of VAT based on easily measurable biomarkers, like those found in blood, is important for future studies of obesity-associated cancer and other diseases," said Le Marchand.
Gut bacteria, colorectal cancer
The second publication, led by Unhee Lim, studied the gut bacteria of MEC Study participants in relation to their levels of a blood marker, trimethylamine N-oxide (TMAO), which is known to be elevated in people who consume more animal products or who are at a higher risk for colorectal cancer. The researchers found that blood TMAO was associated with an abundance of 13 different types of gut bacteria. These included high levels of fusobacterium, an established microbial risk factor for colorectal cancer. In addition, TMAO was related to higher insulin resistance, which often leads to diabetes.
TMAO in humans is produced entirely by gut bacteria that can convert animal food components to TMAO. The researchers reported earlier that red and processed meat is the leading food source for the TMAO precursor, choline, in a typical diet.
"Since red and processed meat consumption is high in certain ethnic groups that have higher incidence rates of colorectal cancer, our study provides insight into a microbial mechanism for colorectal cancer and supports dietary interventions to reduce cancer risk and improve health disparities," said Lim.
Each year, the EGRP Research Highlights showcase a selection of research publications supported by grants in the EGRP grant portfolio. The EGRP funds research in human populations to understand determinants of cancer occurrence and outcomes. The program is the largest funder of cancer epidemiology grants nationally and worldwide, awarding more than 240 grants and cooperative agreements annually.






