Ewing sarcoma is a rare and aggressive childhood bone cancer. For families facing it, the disease is life-altering, and current treatments often come with devastating long-term consequences.
At MUSC Hollings Cancer Center, cancer researcher Casey Langdon, Ph.D., who has a dual appointment at Hollings and the Darby Children's Research Institute at MUSC, is working to develop improved ways to treat this devastating disease. Langdon recently received a St. Baldrick's Foundation Scholar Grant to further those efforts. The grant provides three years of funding to support early-career researchers pursuing bold ideas in childhood cancer.
Toll of current treatments
Langdon's lab is using the award to investigate safer, improved combination therapies for Ewing sarcoma. The ultimate goal is to develop treatments that are more effective against the tumors while sparing healthy tissues.
"These kids are getting high doses of five different chemotherapy drugs, and those can be brutal," Langdon said. "They work for some, but for others, the tumors come back - and in all cases, the side effects can last into adulthood. These treatments save lives, but they may radically change the direction of a child's life in the process."
The treatments have remained largely unchanged for more than 30 years, Langdon said, and as a result, survival rates for children with Ewing sarcoma have also not improved. In contrast, many adult cancers have seen dramatic advances. A major challenge is the rarity of the disease: With only about 250 cases in the U.S. each year, it is difficult to conduct large-scale clinical trials to test new treatments.
"We haven't had much improvement in Ewing sarcoma care in about three decades now. There are just not that many mutations in the cancer cells, so there are fewer targets we can go after. Similarly, Ewing sarcomas don't respond well to immunotherapy because they have fewer mutations that help the immune system recognize cancer."
Going bald with St. Baldrick's
Support from organizations like St. Baldrick's is critical for advancing cancer research, especially for rare cancers. And that support is more than financial - volunteers and supporters offer moral support through events like the annual Lowcountry Bald, where participants shave their heads to raise money for St. Baldrick's.
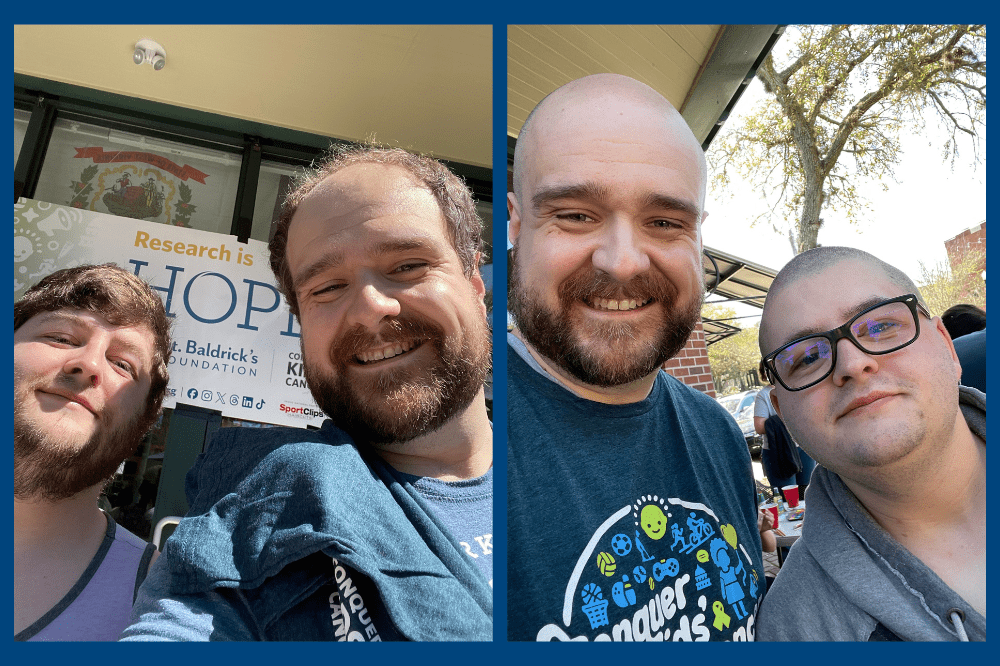
"Choosing to have our heads shaved at the Lowcountry Bald event is our way of honoring kids battling cancer who don't get the choice when they go bald during treatment," said Jamie McKee, a main organizer of the event.
This year, Langdon was one of the shavees, going bald along with Cameron Bumbleburg, a third-year doctoral student in his lab, and Chris Winn from LOWVELO, a fundraiser for Hollings.
McKee appreciates the relationship with Hollings.
"We have been blessed to have Hollings researchers like Casey participate as shavees and share their insights into the progress being made in the battle to conquer childhood cancer," he said.
Targeting cancer's weak spots
Langdon's team is focused on developing combination therapies that exploit unique vulnerabilities in Ewing sarcoma cells. Unlike chemotherapy or radiation, which attack both healthy and cancerous cells, targeted therapies focus on cancer's unique weaknesses.
In the case of Ewing sarcoma, Langdon's lab has found one such weakness: Cancer cells often redistribute proteins to unusual places inside the cells. This misplacement can fuel tumor growth, but it can also create vulnerabilities - much like an "Achilles' heel" - that can be targeted with the right drugs.
"We're interested in how cancer cells shuffle proteins to places they shouldn't be," Langdon explained. "That movement can create vulnerabilities. If you give one drug that forces the cancer cells to rely on a new pathway, and then hit that pathway with a second drug, the combination can be very powerful."
For instance, one of the drugs they are studying blocks the transport of proteins from the nucleus to the cytoplasm within cancer cells. On its own, the drug does not stop tumor growth; rather, it forces the cancer cells to become more reliant on other pathways. By then adding a second drug that blocks those new pathways, the team has seen evidence of synergy, where the drugs together work much better than either one alone.
Langdon's lab is also studying differences between cancer cells within the same tumor - and how those different cells respond to the treatments they are testing. This could help them to refine therapies and to make them more personalized to individual patients.
Moving the research forward
This work is still in its early stages, taking place in cell lines and patient-derived tumor models rather than human patients. But Langdon believes the approach has real promise - not only for Ewing sarcoma but potentially for other hard-to-treat childhood cancers.
"Our ultimate goal is to move this into clinical trials," he said. "If we can one day give these children better, safer options, that would be huge."
Importantly, Langdon's team is testing Food and Drug Administration-approved drugs that block protein misplacement and growth pathways frequently hijacked by cancer cells. Because these drugs have already cleared safety hurdles in treating adult cancers, they could more easily be translated into pediatric trials if they are shown to be effective.
"Every pediatric cancer is technically rare, but the impact is enormous. When a child's life is cut short, society loses decades of potential. Support from organizations like St. Baldrick's helps us pursue the questions that could change that."






