In an Australian first, researchers at the Heart Research Institute (HRI) are using lab-grown 'mini-hearts' as they work to develop a new drug to protect breast cancer patients from potentially life-threatening heart complications caused by chemotherapy.
While breast cancer is the second most commonly diagnosed cancer in Australia, the very treatments helping patients survive, including chemotherapy and antibody-based therapies, are also putting them at increased risk of severe cardiovascular disease.
Now, a team of scientists in HRI's Heart Muscle Laboratory, led by Professor Julie McMullen, are racing to change that.
"We currently have limited knowledge on why cardiotoxicity occurs and which women will be most impacted. This research has the opportunity to identify women at risk of cardiotoxicity before symptoms are present, so we can develop drugs to protect the heart during and after cancer treatment," Prof McMullen said.
HRI researcher Dr Clara Liu Chung Ming is working on the pioneering project using lab-produced 'mini hearts' - tiny, beating spheroids the size of a grain of sand and created from patient blood samples - to test drugs that could one day be safely administered alongside chemotherapy.
"Some women survive breast cancer only to face heart failure, arrhythmias, or other cardiovascular conditions years later which is sometimes even worse than the cancer itself," Dr Liu Chung Ming said.
"Our work is about preventing that, we want to give patients a therapy that can be safely delivered with their cancer treatment, to protect the heart before any damage occurs."

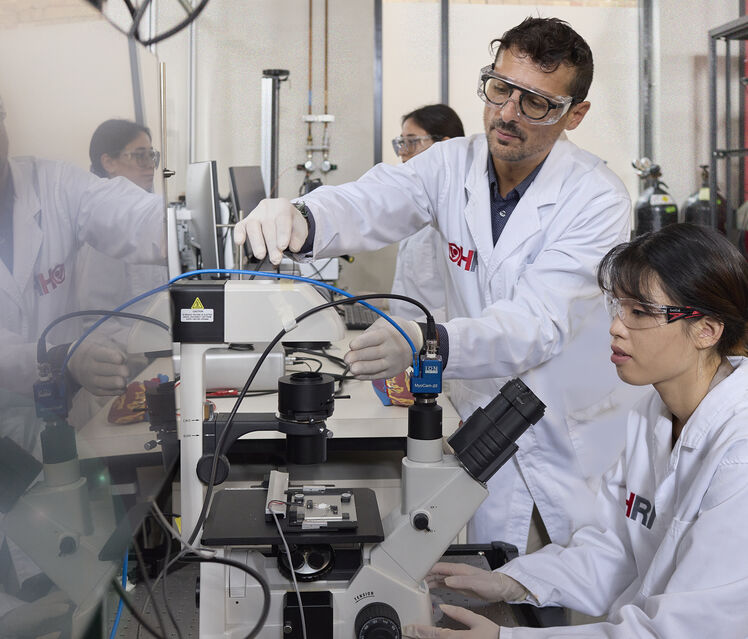
Professor Julie McMullen (left) and Associate Professor Carmine Gentile with Dr Clara Liu Chung Ming (right)
While cancer-related mortality has declined in recent decades, heart disease related to cancer treatment is now emerging as a significant threat. Up to 30 per cent of breast cancer patients treated with chemotherapy may develop cardiac toxicity, with some effects not appearing until five to 20 years after treatment.
Professor McMullen said while the research project is still in the pre-clinical stage, the potential is significant.
Her team has already developed one promising cardioprotective drug candidate and are currently testing it on their patient-derived microscopic 3D 'mini-heart' models that mimic aspects of human heart function. The model was developed in the laboratory of Associate Professor Carmine Gentile (University of Technology Sydney and HRI) who is working closely with Professor McMullen's team.
"Our mini hearts, smaller than a grain of sand, replicate how a real heart contracts and responds to stress. We expose them to chemotherapy and see how they react, then introduce our drug and see if it helps," Liu Chung Ming said.
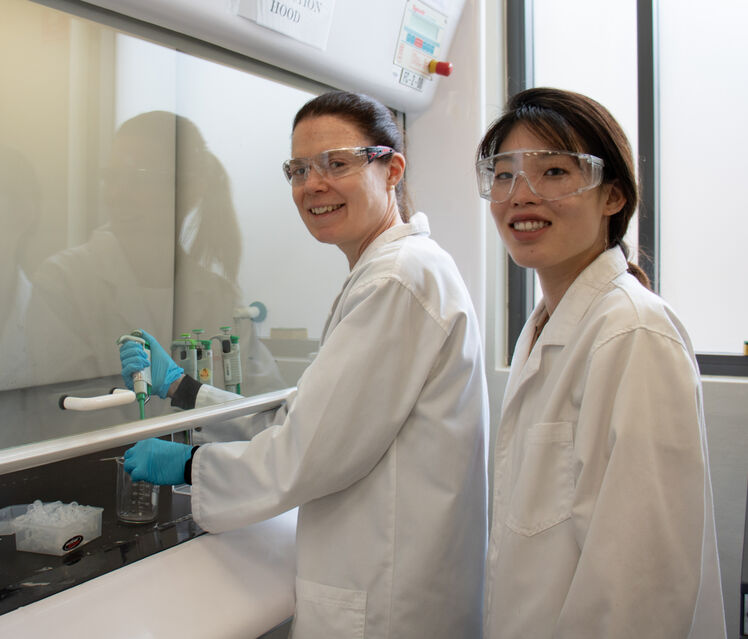
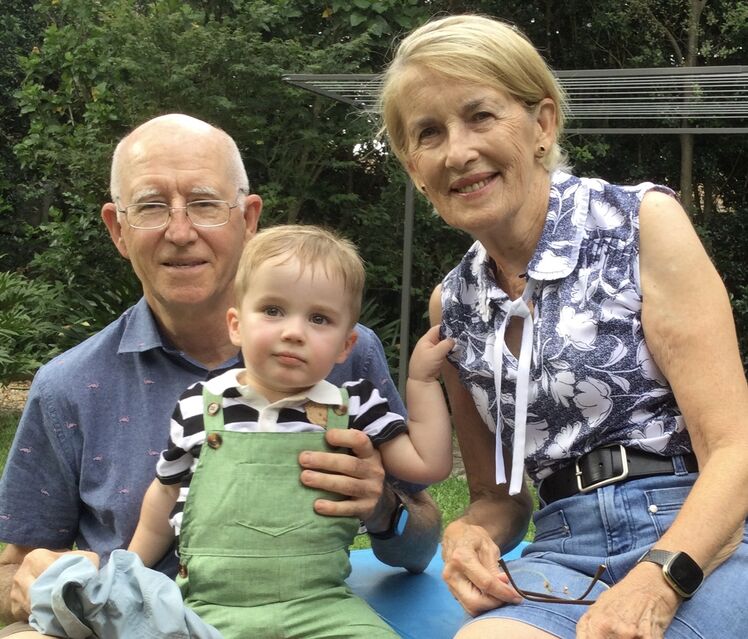
Professor McMullen with Dr Liu (left) and cancer survivor Lee Hunt with her grandson and husband (right)
This research is vital to help people like cancer survivor and advocate Lee Hunt. When Lee was diagnosed with Grade 3 HER2-positive breast cancer in 2005, she hadn't realised that the treatment she was about to undergo carried risk factors for her heart health.
"Then about five years after I finished all my treatments, I started fainting, just out of the blue," Lee says. "It was getting quite more common, suddenly feeling really dizzy ."
Following these fainting spells, Lee went to seek help from her GP, who saw she had high blood pressure and referred her to a haematologist (specialists in blood diseases). When the haematologist learned of Lee's history with cancer, luckily, they knew to send her to seek advice from a cardiologist.
There, Lee found that she experienced reduced heart function as well as long-term cardiotoxicity from her chemotherapy treatment.
"I've had vascular surgery and that did make a big difference, but for other patients, maybe that's not an option," Lee shares. "This research is so important and could save future lives."
The ambitious cardio-oncology project aims not only to identify safer, more effective preventative drugs, but also to understand why some patients are more susceptible to cardiotoxicity than others, helping pave the way for more personalised treatment in the future.
"We're creating a new model to better predict and prevent heart complications in cancer care," Dr Liu Chung Ming said.
"It's about saving hearts as well as lives."
The HRI team is working closely with hospitals including Chris O'Brien Lifehouse and is actively seeking to expand to more centres across Greater Sydney. The next step will be to use breast cancer patient blood samples to generate personalised mini hearts.
Top image caption: Lee Hunt touring the HRI laboratories with Professor McMullen and Dr Liu Chung Ming






