Digestive disorders can affect us all from time to time. Symptoms such as bloating and pain, often accompanied with some change in bowel habits, can be a feature of dietary changes, infection and stress. However, when these symptoms last a long time and no clear cause is found, they can be hard to diagnose and treat.
Author
- Karen Wright
Lecturer in Biomedical and Life Sciences, Lancaster University
Debilitating symptoms, such as fatigue, brain fog, nausea, bloating, gas and flatulence and diarrhoea, can be embarrassing and a struggle to manage. And access to clinical assessment and treatment may not be swift. Googling will probably land you at irritable bowel syndrome (IBS) and self-treating may not address the root cause of the symptoms and could even exacerbate the underlying condition.
This is especially risky with small intestinal bacterial overgrowth (SIBO) because the symptoms are often similar to IBS . SIBO has recently gained more attention through social media and celebrities talking about their experiences with the condition, so what is it and how is it different to IBS?
The clue is in the name. With SIBO, an excessive number of bacteria colonise the small intestine. In contrast, IBS is a condition with many causes. The body becomes more sensitive to pain in the stomach and intestines. Symptoms include immune system activation, abnormal gut movement, changes in gut microbes and disruptions in the gut-brain axis .
The gut-brain axis is the communication system between your digestive system and your brain. These two are constantly sending signals to each other through nerves, hormones and even gut bacteria - like a two-way radio line that helps manage things like digestion, mood and stress.
Both IBS and SIBO may be associated with psychological symptoms , such as anxiety, depression, stress and reduced quality of life.
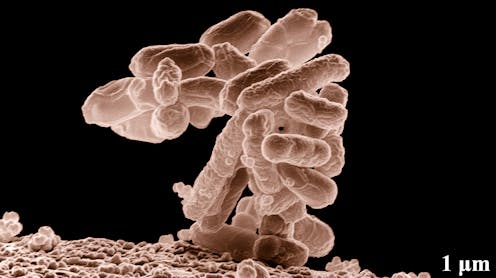
Most of your gut bacteria should live in the large intestine (the colon). The small intestine, especially the upper part (the duodenum and jejunum), has much fewer bacteria.
With SIBO, bacteria that are supposed to stay in the large intestine migrate up into the small intestine - particularly after surgery or if the movement of food through the intestines is slow - or bacteria in the small intestine start growing excessively.
Coliform bacteria, usually found in the colon where they help ferment carbohydrates, can enter into the small intestine and expand their numbers. The fermentation produces gas, which gets trapped and causes bloating and pain. This can lead to belching and flatulence , along with nausea and diarrhoea.
Most of the time, stomach acid minimises bacterial entry to the small intestine, but many people suffer from acid reflux or stomach ulcers and use proton pump inhibitors (PPI). These are medicines, such as omeprazole, lansoprazole and pantoprazole, that reduce stomach acid production.
Prolonged use of PPIs can disrupt the digestive system's natural defences, impair gut motility and alter the microbiome - all of which increase the risk of developing SIBO.
Slow movement of food can be the result of disrupted nerve signalling to the muscles - sometimes seen in diabetics. Also, some medicines or narcotic drugs can slow gut motility, too. Both provide opportunities for bacteria to expand in the wrong place.
Equally, slow movement of food from the small to large intestine, from ageing or surgery, can allow bacteria to enter the wrong place - where they're still able to expand and ferment food causing gas, bloating and discomfort.
Symptom overlap
Can IBS cause SIBO or vice versa? Symptom overlap can lead to misdiagnosis and diagnostic approaches differ. The gold standard for SIBO diagnosis is a rather invasive collection of a small sample from the small intestine. This sample is then cultured to identify the culprit bacteria.
There are two simpler breath tests, which are controversial in their reliability . IBS diagnosis requires the exclusion of other diseases - such as the inflammatory bowel diseases, Crohn's disease or ulcerative colitis - as well an analysis of the symptoms such as frequency of bowel movements and pain recurrence, combined with blood and stool tests.
Meta-analyses of pooled data indicates 25%-36% of IBS patients have SIBO. SIBO may contribute to IBS symptoms or be a consequence of IBS-related motility issues.
However, underlying both of these conditions is a dysregulated gut microbiome. This is when the normal balance of microorganisms in your digestive tract - mainly bacteria, but also viruses, fungi and other microbes - gets disrupted in a way that can lead to health problems, including psychological issues.
The gut and brain are connected through a two-way communication system known as the gut-brain axis, which is influenced by the microbes in the gut. When this microbial balance is disrupted, it can contribute to mental health issues like anxiety and depression.
Although antibiotics are used for treating SIBO, use is not desirable because it can lead to antibiotic resistance, disruption of the gut microbiome and the condition could recur once the antibiotics are stopped.
Long-term antibiotic use can also lead to side effects like gastrointestinal issues, yeast infections and damage to the intestinal lining. What's more, antibiotics don't address the underlying causes of SIBO, such as motility issues or structural problems in the small intestine.
Drugs that increase gut motility are useful to prevent SIBO recurrence and are used in IBS where there are motility symptoms. Elemental diets , which reduce available carbohydrates for bacterial fermentation, have been shown to be effective for both IBS and SIBO.
Modifying the gut microbiome through diet, probiotics, and other approaches may provide new ways to treat and manage these conditions. Therapeutic strategies that restore the balance of gut bacteria could also help restore a healthy gut-brain connection, potentially improving mental health.
![]()
Karen Wright is affiliated with Cannabinoid Research and Development Group UK.






