With its many variations, its ability to mutate, evade population immunity, and spread throughout the population, and its potential to cause serious illness and even death, the influenza viruses are worthy adversaries. In a summer blockbuster movie, the flu would be the supervillain.
Fortunately, a team of avengers has assembled at Johns Hopkins University, partner universities across the country, and research sites worldwide. They bring qualities similar to the viruses they are battling—varied in skill and specialty, nimble and flexible to respond to new challenges, and powerful enough, both individually and as a collective—to use research to advance the knowledge of and response to influenza and other respiratory illnesses.
The Johns Hopkins Center of Excellence for Influenza Research and Response, or JH-CEIRR, is one of six such centers in the country. They are funded by the National Institute of Allergy and Infectious Diseases, or NIAID, part of the National Institutes of Health, and were created to study influenza and combat influenza outbreaks.
JH-CEIRR is a global network of research sites studying many facets of influenza and other infectious diseases, including the genomic characteristics of viruses, how they evolve, how they infect, how they transmit in patients, and immunological and vaccine responses. The data and findings not only help with patient care but help organizations like the NIAID, NIH, CDC, and others, including large health systems and government agencies, with public health preparedness and response.
Thanks to the work of JH-CEIRR and its team of researchers in Baltimore and elsewhere, we can better understand the behavior of the virus, improve treatment, manage seasonal outbreaks, and keep more people safe and healthy.
One of the strengths of the Johns Hopkins team is its multi-disciplinary approach, says emergency medicine expert Richard Rothman, who serves as JH-CEIRR co-director along with Andy Pekosz, a virologist and professor at the Johns Hopkins Bloomberg School of Public Health.
"There is a partnership between the School of Medicine and School of Public Health, which brings together clinicians and epidemiologists, along with experts in molecular biology, virology, diagnostics, and public health," Rothman said. "We're able to look across the whole spectrum of care, from the cellular level to individual patients to improving public health."
Pekosz and Rothman began directing the Hopkins CEIRR program in 2014 and completed seven years of research before renewing a funding grant for another seven. JH-CEIRR is nearing the end of year four of that second seven-year period. Funding from the NIH for year five started in August, though the current political climate in Washington, D.C., has added uncertainty to the federal research funding landscape. While Pekosz said the team seeks other means of funding, the overwhelming majority of the center's nearly $5 million annual budget comes from NIH.
Funding not only supports the work at Johns Hopkins, where six other investigators are part of the center, but also at eight partner universities across the country: Montana State University, Ohio State University, the University of Colorado, the University of Missouri, Boston University, Cornell University, New York University, and the University of California-Santa Cruz. At Montana State, for example, investigator Emma Loveday said CEIRR grants have allowed her to establish a research lab and support five additional employees.

While there are obvious employment and economic benefits that come from the funding, the primary focus of the team's work is the lifesaving scientific research they are conducting.
The work is as varied as the various researchers' backgrounds, interests, and areas of expertise, spanning genomic sequencing, diagnostics, public health data, and more.
Understanding the virus
Influenza affects about 8% of the U.S. population annually, according to the CDC. It can cause mild to severe respiratory illness, and at times can lead to death. Flu season typically peaks in the winter in the U.S. and varies in severity from year to year, with some patients getting less sick and other suffering serious health consequences. In some years, up to 50,000 related deaths occur. Health experts say the annual flu vaccine is the best way to prevent the flu.
The influenza virus has four types—A, B, C, and D—with A and B the ones known to cause seasonal epidemics in humans. Within each type are subtypes or lineages; for influenza A, the subtypes are based on the two proteins on the surface of the virus: hemagglutinin (H) and neuraminidase (N). That's where names for common flu types such as H1N1 come from. Scientists can break down subtypes further into groups known as clades and sub-clades, as well as determine the sequence of the nucleotides in the virus's genes. Heba Mostafa, associate professor of pathology at the Johns Hopkins School of Medicine, runs the medical microbiology diagnostic lab at Hopkins and does most of the sequencing for JH-CEIRR.
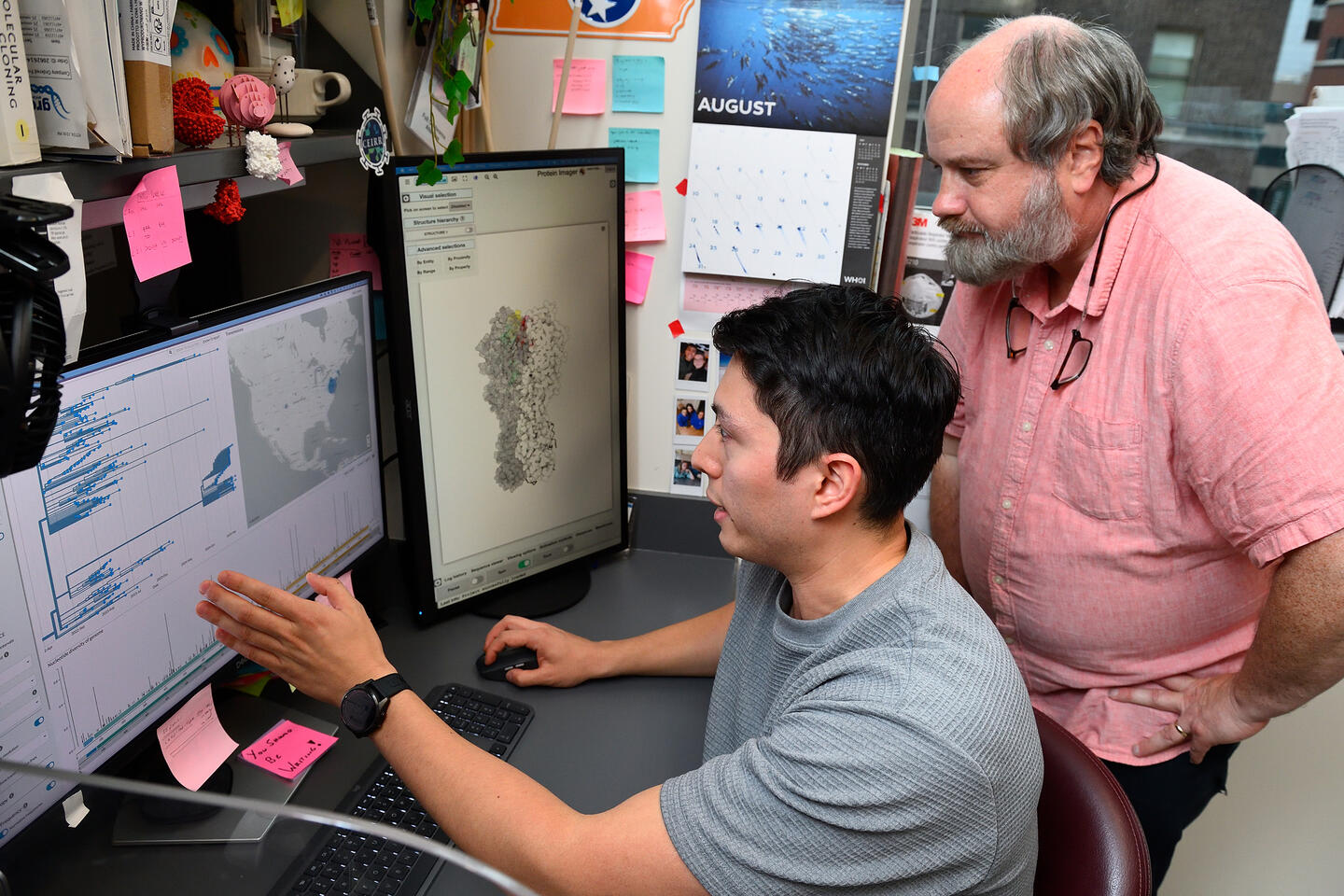
Image credit: Will Kirk / Johns Hopkins University
Genomic sequencing allows researchers to characterize each virus and compare it to others. Variations between viruses can be critical to understanding their severity and impact.
"In our labs, we characterize the viruses that are circulating so we can understand the mutations in the viruses, how they might change the ability of the virus to cause disease, and then, importantly, how vaccines would recognize the viruses that were circulating," Pekosz said.
Understanding the differences in viruses has tremendous public health benefit, Pekosz said.
"We often can predict, just from a few sequences of the virus, whether there's been a major change from last year's virus, and that we should expect something different in a flu season," he said. "We can see if we've seen a certain mutation before and understand if that correlates with more disease potential. All of that helps with planning. It helps our hospitals prepare. It helps prepare our public health response."
In addition to the real-time sequencing at Johns Hopkins, Loveday in her lab at Montana State uses microfluidic technology to study individual cells infected with the virus. This provides critical fundamental knowledge about viral behavior that could inform future vaccine and treatment strategies.
Jenna Guthmiller's work at the University of Colorado Anschutz Medical Campus is funded by a grant through JH-CEIRR that started in fall 2023. She and her team focus on understanding antigenic drift in influenza viruses. Antigenic drift is the process in which small changes in the proteins of a virus affect the immune system's response. Guthmiller also investigates how the immune system and antibodies respond to these viral changes, which can inform future vaccine development and pandemic preparedness.
"The grant catapulted our research forward," Guthmiller said. The grant was for about $325,000 covering two years, meaning its future as of later this year is up in the air.
Surveillance and response
CEIRR was originally CEIRS, with the S standing for surveillance, before it was changed to response. Despite the change, researchers still do both.
"We have brought resources at the front lines of the health care system and other capabilities that exist at Johns Hopkins to better understand emerging threats," Rothman said. "Through the work from the center we have built improved capabilities for diagnostics, situational awareness, public health surveillance, and overall health system response."
JH-CEIRR has three surveillance sites: in Baltimore, Taiwan, and Macha, Zambia. Macha is a very rural area and is also in the Southern Hemisphere, so it can provide data that may look very different from other sites, according to Catherine Sutcliffe, research professor at JHU's Bloomberg School and one of the primary people collecting and analyzing data on influenza and other respiratory viruses circulating in Macha.
Adds Pekosz: "We try to capture all the different facets of influenza virus and respiratory virus infection through these three surveillance sites."
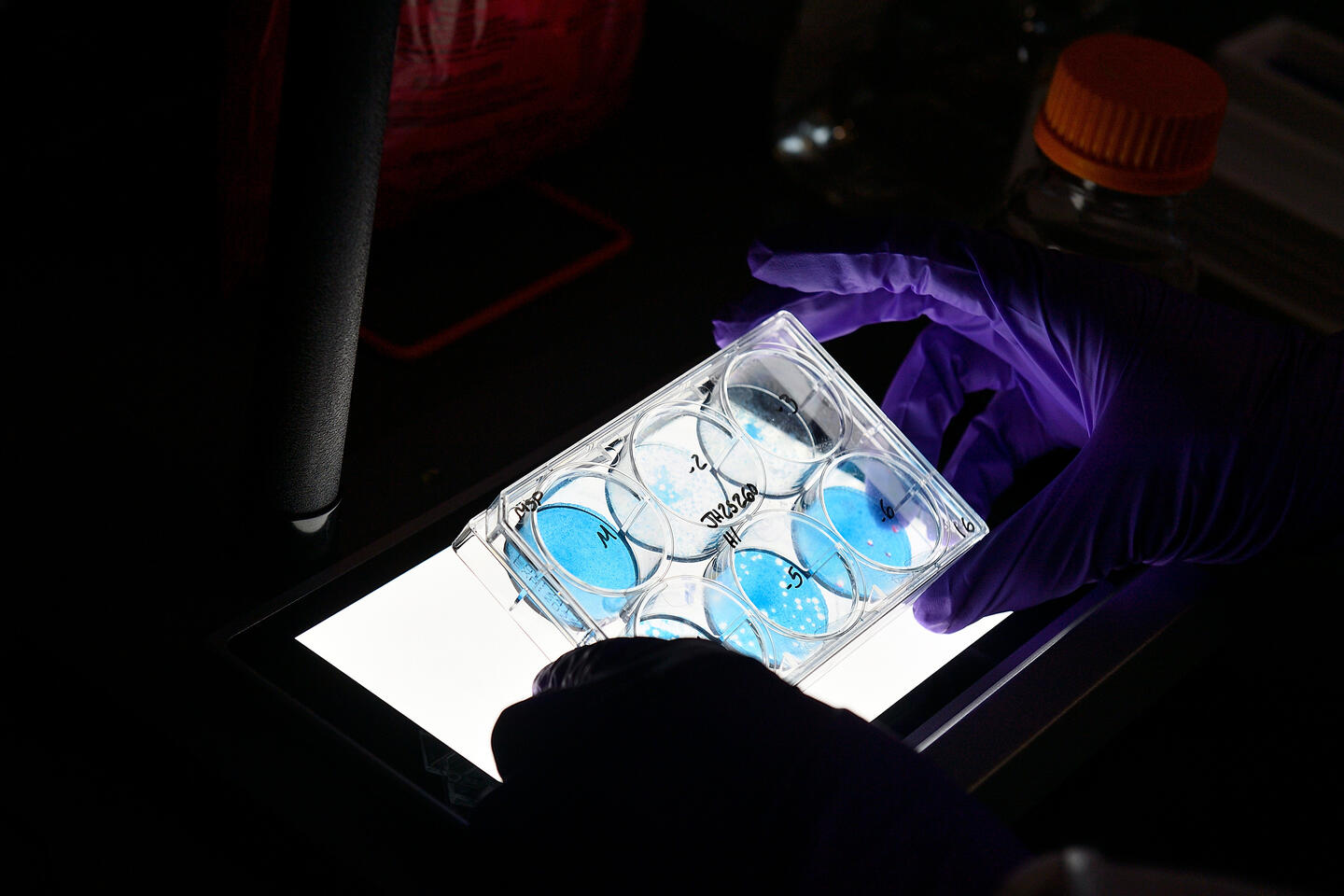
Image credit: Will Kirk / Johns Hopkins University
Other research includes studying different ways individuals respond to the virus or vaccines, as well as better diagnostic tools. For example, Sabra Klein, professor in JHU's Department of Molecular Microbiology and Immunology, has shown that sex hormones more so than age affect vaccine effectiveness—particularly the presence of estrogen helping response and the presence of testosterone hindering it. In addition, Pekosz said, there's work at the University of Colorado that has shown the year in which you are born can sometimes dictate your response to influenza.
Researchers also have created and are now testing better diagnostic tools, Rothman said, which not only improve accuracy, but can help recognize new or emerging strains earlier than traditional methods. Innovation in testing methods have been bolstered through the recently constructed Emergency Department Clinical Innovation Center, which focuses on bringing point of care testing methods for influenza and other respiratory viruses closer to the patient.
Other capabilities advanced through CEIRR include using AI tools to better predict which patients infected with influenza may need more intensive medical resources, such as ICU-level care. This work is being pushed forward through a CEIRR award to help support collaborative work with Jeremiah Hinson and Eili Klein, both associate professors in the Department of Emergency Medicine at Hopkins.
Impact on vaccinations
Vaccines are tremendously important in preventing flu and mitigating outbreaks. Much of the CEIRR's research can lead to more effective vaccines and a better understanding of how the virus is able to evade a vaccine.
"The knowledge we gain from sequencing the viruses can inform the selection of the vaccine strain for the next season," Mostafa said.
Katherine Fenstermacher, executive director at JH-CEIRR, said the center is observing people who are already receiving annual flu vaccines to understand things like what biological factors affect vaccine effectiveness and what rates of vaccination are most effective. Scientists at Boston University that are part of JH-CEIRR are combining vaccine data and machine learning to predict future vaccine responses, Pekosz said.
Pandemic preparedness
"CEIRR networks are put in place first to gain a better understanding about respiratory viruses and their normal circulation, but also to use that as a platform to help prepare for a pandemic," Pekosz said. "With influenza, we're expect that at some point in time we'll have another pandemic."
A pandemic did emerge amid their work, but it wasn't influenza. Still, the infrastructure and expertise in place allowed CEIRR researchers to pivot and become among the earliest to study, diagnose, and respond to the COVID-19 pandemic, which was caused by a different respiratory virus.
Mostafa's lab, for example, was able to characterize the first instances of the coronavirus omicron variant in 2021 and provide guidance for treatment based on the data.
Additional research on antigen tests correlated results with the amount of infectious virus in nasal samples, which informed the CDC's decision to shorten their recommended isolation periods after positive tests—allowing people to return to work in five or six days instead of two or three weeks.
"Since our team had experience with respiratory pathogens, we were poised to be this really rapid response to a pandemic," Fenstermacher said. "And that's continued. We are now facing the threat of bovine H5N1 influenza, and we've put into place pathways where our team can respond very quickly."
Loveday at Montana State has in fact shifted some of her research in response to the bovine H5N1 flu outbreak that began last year.
"We pivoted to try and provide answers, perspective, and data on what was happening with H5N1 as quickly as possible," she said. "We used existing tools from our CEIRR work to understand what this H5N1 was doing, to learn if it could infect human cells and how it was happening. That information from different CEIRR centers filtered through the government to provide critical information as fast as possible. The value of that I don't think can be overstated."






