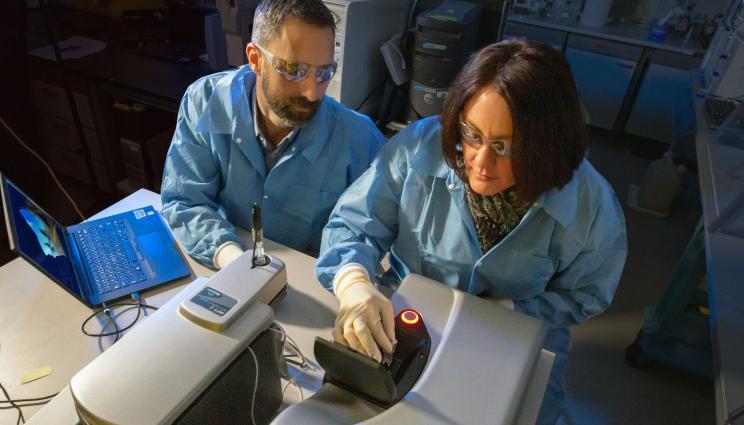
LLNL researchers Nick Fischer and Amy Rasley are characterizing nanolipoprotein particle vaccine formulations using a dynamic light-scattering instrument. Detailed characterization of the nanoparticles provides an important quality control metric for vaccine development. Photo by Julie Russell/LLNL
Two Lawrence Livermore National Laboratory (LLNL) researchers who have worked for more than eight years to develop a tularemia vaccine are part of a three-institution team that has been funded to bring their candidate to readiness for use.
The two biomedical scientists, Nick Fischer and Amy Rasley, will collaborate with scientists from the University of New Mexico and the Tulane National Primate Research Center under a five-year, $7.5 million grant from the Defense Threat Reduction Agency (DTRA).
Using the candidate vaccine, the LLNL scientists have demonstrated the ability of a subunit vaccine, incorporating different antigens from the Francisella tularensis bacteria into a single particle, to protect against high doses of this bacteria when aerosolized. F. tularensis is the bacteria that causes the disease tularemia, more commonly known as rabbit fever.
"This demonstration is only a first step, but it is a critical advance that researchers have been trying to achieve for more than three decades," Rasley said.
"We had confidence that we could develop a tularemia vaccine that would work," said Nick Fischer, "but it took eight years of hard work and multiple failures to get us where we are today."
Kris Kulp, the acting leader for the Lab's Biosciences and Biotechnology Division, said LLNL is "tremendously proud and excited" to be part of the effort to develop a vaccine that could protect soldiers and civilians from tularemia, a high-priority pathogen.
"This project leverages expertise our scientists have worked hard to perfect and highlights our ability to contribute to the Lab's national security mission. The collaborations formed with our university partners are key to producing and testing this novel vaccine. We anticipate this project will significantly enhance our nation's ability to protect our soldiers," Kulp said.
The three-institution project will be led by Terry Wu, a tularemia expert, and by the University of New Mexico Health Sciences Center (UNM HSC).
"This project is the culmination of almost 20 years of research funded by DTRA and the National Institute of Allergy and Infectious Disease since the terrorist attack in 2001," Wu said. "UNM HSC researchers will work closely with collaborators at LLNL and Tulane University on pre-clinical studies required to advance the vaccine toward clinical use."
The scientists will build on a nanotechnology - called nanolipoprotein particles (NLPs) - that was developed at LLNL for delivering vaccines and drugs inside the human body.
NLPs are water-soluble molecules that are 6 to 30 billionths of a meter in size and resemble HDL particles, which are associated with playing a role in regulating the human body's good cholesterol. LLNL scientists have worked on this nanotechnology, also known as nanodisc, since 2005.
Using the NLPs as a delivery platform, the F. tularensis antigens can be co-delivered with an adjuvant molecule, which stimulates the immune response against the antigens. LLNL, in partnership with UNM, has identified the correct combination of antigen and adjuvant.
When co-localized on the NLP and delivered as a vaccine, the formulation was able to protect against aerosolized tularemia at levels well beyond what was expected from a subunit vaccine, Fischer said.
There have been a number of successful efforts to develop tularemia vaccines using live, attenuated strains of F. tularensis, but there are often risks associated with using such strains of a bacteria, Rasley said.
"The profile for subunit vaccines is significantly safer than for using live, attenuated strains," Rasley said. "But the tradeoff for that safety is often a less effective vaccine. Our focus has been to enhance the efficacy of the subunit vaccine by inducing a protective immune response. This is where the NLP platform was instrumental in the development of our subunit vaccine because it serves as a delivery tool for the antigens."
Lab researchers see the NLPs platform as a flexible tool that can broadly be applied to developing vaccines for different pathogens.
In October, LLNL announced that the National Institutes of Health had established a cooperative research center at Livermore under a five-year, $10.1 million grant to develop vaccines for chlamydia. The center includes researchers from two University of California campuses - Irvine and Davis.
Under the five-year DTRA grant to develop a tularemia vaccine, LLNL researchers are expected to receive $3.6 million to conduct their work.
The goals of the DTRA project are to validate the preliminary data, test the vaccine's ability to protect in more rigorous models and optimize the production and scale-up of the vaccine formulation.
F. tularensis is classified as a class A high-priority pathogen and select agent by the Centers for Disease Control and Prevention. It is considered a potential biothreat agent based on its extremely low infectious dose.Disease manifestations vary depending on the route of exposure. It is an infectious disease that can cause fever, skin ulcers, enlarged lymph nodes, pneumonia and throat infection with inhalational disease (pulmonary tularemia) being most severe.
In addition to Fischer and Rasley, other LLNL biomedical scientists who are part of the team working to develop a tularemia vaccine are Sean Gilmore and Sandra Peters.






