Multicenter examination showed biomarkers in cerebrospinal fluid consistently distinguished MS from other conditions
Cerebral-spinal fluid (CSF)-based molecular tests can reliably distinguish multiple sclerosis (MS) from other neurological conditions, according to a study that analyzed cryopreserved CSF samples from 160 individuals.
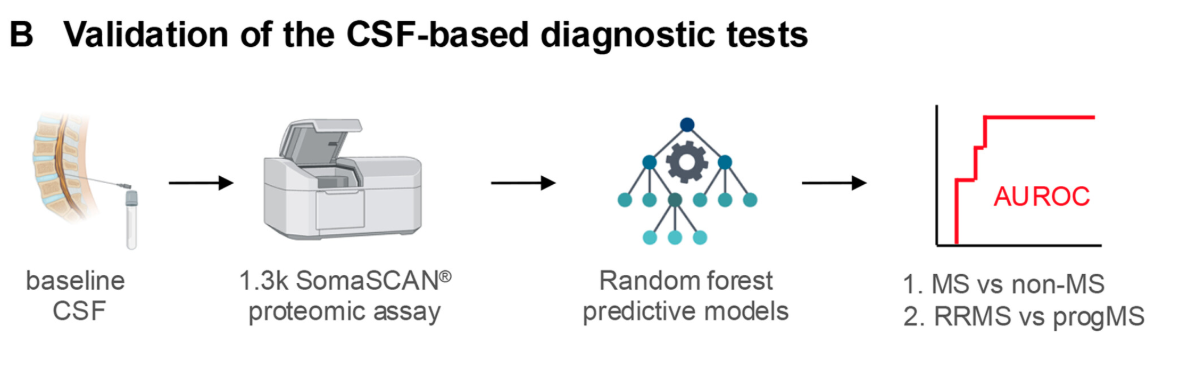
The study involved three centers in the United States and Canada that are part of a MS research consortium called SPINCOMS. The group evaluates the clinical performance of CSF-based molecular tests in a diverse cohort of people with MS and others undergoing diagnostics for central nervous system conditions that mimic MS.
"The consortium allowed us to go back and look at spinal fluids that had been collected in the past (between 1988 and 2019), and to try to validate previously-done testing to answer a couple questions," said study co-author Enrique Alvarez, MD, PhD, professor of neurology at CU Anschutz. "One was: Could we predict who had MS versus those who didn't? And then another was, within those who had MS (96 of the 160 samples were clinically confirmed), could we stratify the people who had progressive MS versus relapsing MS?"
Researchers also analyzed the data to see if they could predict the level of disability progression.
Advancing personalized care
Previous studies at the National Institutes of Health found the potential of CSF biomarker-based models to improve MS diagnosis. This study, published in the Annals of Neurology, extended to multiple centers, showing that these CSF molecular biomarkers can consistently distinguish MS from other conditions and provide information about disease progression. The results help lay the groundwork for next-generation personalized treatments.
Key points:
Nearly 1 million people in the United States and 2.8 million worldwide live with multiple sclerosis (MS).
Clinical diagnoses of neurological disorders have an estimated error rate of 20% to 40%.
Cerebral-spinal fluid-based molecular tests can reliably distinguish MS from other neurological conditions.
Nearly 1 million people in the United States and 2.8 million worldwide live with MS. The disease damages nerves, disrupting signals between the brain and the rest of the body. The disease, which has no cure, presents in stages: relapse-remitting MS (RRMS), the most common form, with symptoms arriving in intermittent flares; and progressive MS (progMS), with subsets of secondary-progressive, primary-progressive and progressive-relapsing.
Misdiagnosis is a problem with MS because the disease looks different from patient to patient and the route to diagnosis is varied. While misdiagnosis often delays needed treatment, it also exposes some patients to ineffective or unnecessary therapies.
The tests in this study used a multiplex proteomic platform called SomaScan. The technology provides a measure of thousands of different proteins at once, allowing a broad picture of biomarkers.
According to the recent study, clinical diagnoses of neurological disorders have an estimated error rate of 20% to 40%. Similar diagnostic uncertainties exist for the current standard diagnostics for MS - magnetic resonance imaging (MRI) and clinical assessments. Three of the 96 samples clinically classified as MS were not consistent with MS using this testing. In retrospect, these three had "red flags" that questioned the diagnosis of MS.
"If you can diagnose it earlier, you can treat the patients earlier," Alvarez said. "Especially from a relapsing stage perspective, we have very effective drugs. So, if we can stop those relapses, we can really reduce disease accumulation in these patients. In the field, it's thought that if we can do that early, we might even prevent patients from going into the progressive phase."
Answering the study questions
On the question of how the CSF-based molecular diagnostic test differentiates MS from other neurological diseases, the study used a probability model where a 1.0 represents perfect accuracy and 0.5 is no better than random guessing. The classifier test achieved 0.94 accuracy.
If only traditional CSF-based MS biomarkers such as immunoglobulinG (IgG) index and oligoclonal bands were examined, Alvarez said, the testing accuracy dropped to 0.82. "So, this neurological differentiator test added another 0.1 of accuracy - making it that much better."
On the study's second question - can the people with MS be stratified into those who have progressive versus relapsing forms of MS? - the model came in at 0.76, with a median predicted probability of 0.78 for individuals with progressive MS and 0.47 with relapsing MS.
On the question of whether researchers could predict the level of disability accumulation, the test did not add as much, but it was still better than scientists' current ability to predict progression.
Seeking more therapies for progressive MS
While many therapeutics have been developed to treat relapsing MS, medicine lags for the progressive stage. The Food and Drug Administration in 2017 approved ocrelizumab as the first medication to treat primary-progressive MS. "We may be seeing other medications get approved with initial indications that Fenebrutinib could be approved in 2027," Alvarez said.
Molecular-based personalized care is a key area of future MS research, according to Alvarez.
"With MS, there is the relapsing variety, and then progression. Progression is very slow, very gradual," he said. "If you can treat the acute relapses, then what you're left with is this progression." So being able to identify who is going to have a progressive phenotype will allow clinicians to, as more drugs are developed to treat progressive MS, better tailor therapies to individual patients.






