As a worldwide pandemic washes over the St. Louis region, the Washington University Medical Campus is eerily quiet. Most visitors, students, staff and research faculty are no longer on campus. Limited patients come to its medical buildings, as many appointments are taking place virtually on video screens.
But it's another story in the COVID-19 wards of Barnes-Jewish Hospital (BJH), where Washington University physicians are fighting an exhausting battle against a new, baffling and sometimes lethal disease with the help of the hospital's nurses, other medical professionals and support staff.

"When the very first suspected COVID-19 patient was admitted to our hospital in early March, I volunteered to take care of him," said hospitalist Han Li, MD, an instructor in Washington University's Division of Hospital Medicine. "And then, we went just from that one patient to the next day having two, three and then more than 100 patients on our floors. We have all been thrown into the fray, and we're focused on figuring out how to get every patient the care they need. There are no firm guidelines because it's a completely new disease, but we are learning new information almost daily. I think we're going to look back on this in a few months, and only then will we have the time to really process things and reflect."
Long before the first case was diagnosed in the St. Louis region, Washington University physicians and BJH started preparing, with support from BJC HealthCare.
"In January, before the United States felt any impact from the coronavirus, we worked with BJH and BJC to start planning how we would care for patients with COVID-19 - specifically, where we would care for them, who would provide that care, how we would outfit our health-care workers with personal protective equipment - so when the number of patients started to surge in March, we could handle it," said William G. Powderly, MD, the Dr. J. William Campbell Professor of Medicine and co-director of the Division of Infectious Diseases. "We had very little information in the beginning about how to treat this disease, so our physicians had to think on their feet when the answers weren't available through limited existing research and clinical accounts of others confronting the virus. The creativity, flexibility and dedication our health-care providers have shown in the face of this novel and sometimes deadly virus has been extraordinary. They are true heroes."
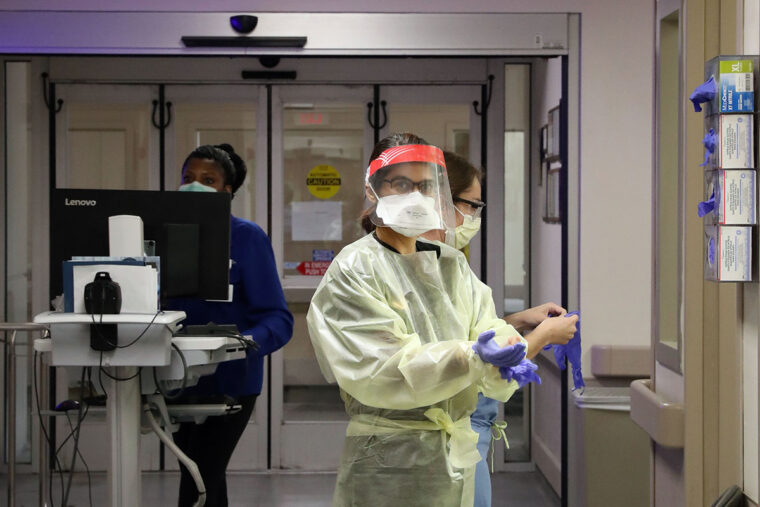
Several specific areas of the hospital and five intensive care units were dedicated to COVID-19. BJC and university logisticians obtained massive quantities of personal protective equipment (PPE) such as masks, gowns, face shields, gloves and goggles for front-line medical staff. Hospital managers shuffled work schedules so there would be enough attending physicians from the divisions of general medicine, infectious diseases, and pulmonary and critical care available to care for the dozens of cases expected to arrive.
"Because of all the planning, the workload has been manageable, but the actual work is much more difficult than usual," said Komo Gursahani, MD, an associate professor of emergency medicine at the School of Medicine and assistant director of the BJH emergency department. "Just the donning and doffing of personal protective equipment repeatedly can add a lot of stress because we have to be very careful with how we put the equipment on and remove it so we don't contaminate ourselves. And we have to be cognizant that every test we order - whether it's X-rays or CT scans or some other diagnostic - requires someone to have contact with the patient. So every decision we make now comes with a little added factoring in of how much we're exposing our colleagues and coworkers to potential disease."
To minimize the number of health-care workers exposed to the virus, most medical trainees at BJH - interns, residents and fellows - have been redeployed to care for other patients, and care teams have been pared down. Where six people previously might have entered a room to check on a patient, now only two or three go in.
In the early days of the pandemic, doctors thought that the majority of COVID-19 patients who became critically ill had developed acute respiratory distress syndrome (ARDS). ARDS can be triggered by a variety of infectious and noninfectious causes. The condition is very serious, but pulmonary and critical care physicians have been trained to treat it. As the number of cases grew, however, doctors around the world began to realize that not all COVID-19 patients' respiratory symptoms looked like ARDS. And the doctors started to note other complications. Some patients developed heart problems and died of cardiac arrest. Some were caught in a "cytokine storm," which occurs when their own immune systems overreact to infection and produce disastrously high levels of immune proteins. Some developed unusual blood-clotting problems that were hard to detect and treat. Clots are very dangerous because they can block blood vessels, leading to respiratory failure, heart attacks, strokes, kidney damage and other serious complications. Some patients developed strokes, seizures, confusion or other neurological problems. In short, COVID-19 was unlike any virus they had seen before.
To handle a disease of this complexity, doctors rely on a team of BJH nurses, respiratory therapists and other medical professionals who provide much of the day-to-day care for COVID-19 patients, and a large team of specialists who help guide the care. A multidisciplinary COVID-19 critical care task force that includes physicians from pulmonary medicine, emergency medicine, surgery, cardiology, anesthesiology, neurology, medical ethics and other fields has been set up to make recommendations for patient care. Every day, the intensive care physicians caring for COVID-19 patients meet with specialists in infectious diseases, pulmonary and critical care medicine, nephrology (kidneys), cardiology and other fields for 90 minutes to discuss the care of each of the critically ill COVID-19 patients.
"The information on COVID is always changing and always increasing," said Colleen McEvoy, MD,






