Immunotherapy, which harnesses our body's own immune system to fight cancer, has revolutionized modern oncology. Yet despite its success with several cancers, many patients still fail to respond to therapy or experience relapse later on. Scientists have long sought ways to pinpoint how cancer shuts down the immune response, and to flip the switch back on right at that site. A new study from the Weizmann Institute of Science, published today in Cell , suggests that the solution might lie within the tumor's own defenses. The study focuses on macrophages - large, versatile cells that perform essential functions throughout body tissues but, when found in the tumor microenvironment, often begin collaborating with the cancer. "For years we have known that in cancer, macrophages can be both the problem and the solution," says Prof. Ido Amit , director of Weizmann's Immunotherapy Research Center. "Tumors hijack them to suppress immune responses and promote their own growth. Our goal has been to re-educate these cells rather than remove them."

In earlier studies, Amit's team and others had identified a subgroup of macrophages-turned-tumor-allies that are particularly involved in suppressing the immune response against cancer. Their defining feature is the unusually high expression of a receptor called TREM2, which coordinates their anti-immune activity. Patients whose tumors team up with these macrophages do not respond well to treatment and tend to have lower survival rates.
In the new study, a team led by Michelle von Locquenghien, Dr. Pascale Zwicky and Dr. Ken Xie from Amit's lab designed biological molecules intended to guide wayward macrophages back on track: a new type of antibodies that awaken the patient's anti-tumor immunity by simultaneously blocking TREM2-expressing macrophages and prompting other immune cells to attack the cancer. The latter is achieved by exposing the immune cells to an activating protein called a cytokine. The researchers called this new class of immune-activating molecules MiTEs (short for Myeloid-targeted immunocytokines and natural killer/T-cell Enhancers).
""These molecules are designed to turn both the tumor's allies and its suppressive environment into its Achilles' heel"
A key challenge was avoiding severe side effects: When the immune system is activated too strongly across the entire body, it cannot always tell friend from foe, and can destroy healthy tissue as well as tumors. To prevent this from happening, the researchers resorted to a clever engineering strategy. They managed to equip MiTEs with built-in molecular masks that keep the activating component, the IL-2 cytokine, silent while the molecules circulate in the body on their way to the tumor. Only when MiTEs enter the tumor is this molecular mask removed by special enzymes found only at the tumor site, enabling the cytokine to be activated where it is needed - so that the immune response is unleashed exclusively within tumors.

"The dual function of MiTEs enables them to attack the tumor from multiple immune angles at once," explains von Locquenghien. "These molecules are designed to turn both the tumor's allies and its suppressive environment into its Achilles' heel."
Zwicky highlights the promise of this approach for improving cancer treatment, especially since it acts through immune pathways common to many cancers rather than through tumor-specific antigens. "Because MiTEs act through immune mechanisms present in many patients and cancer types, they have the potential to be broadly applicable," she says.
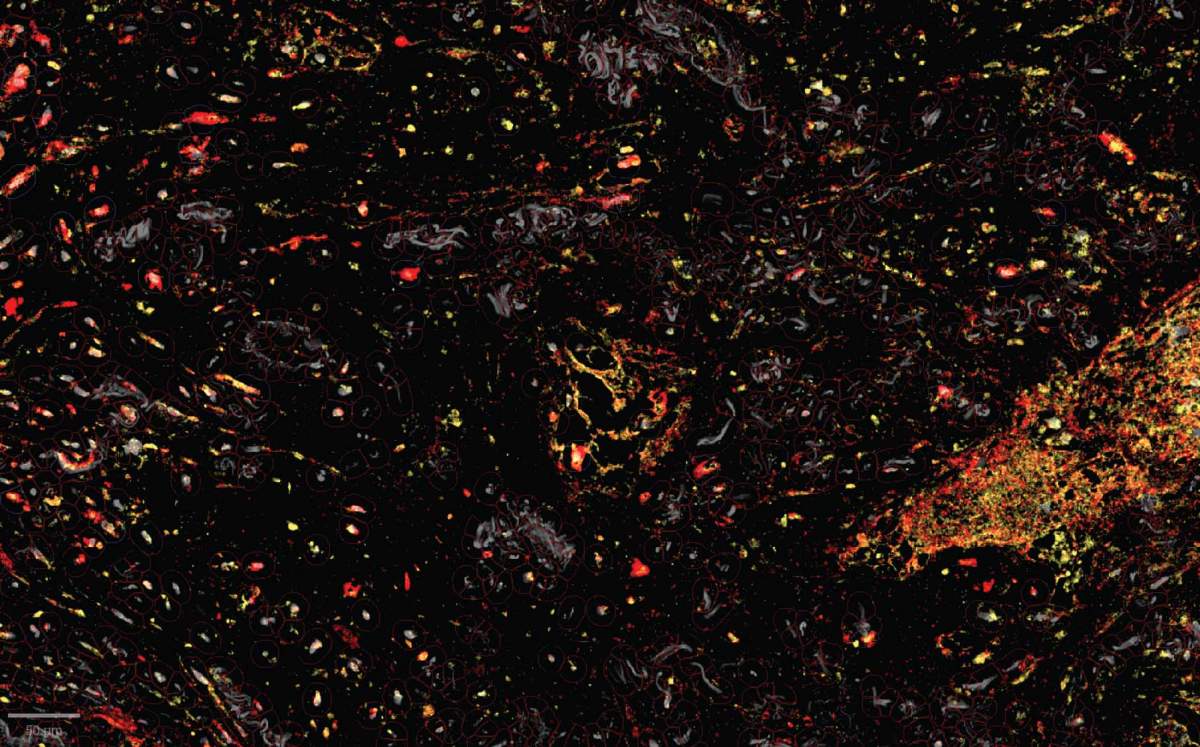
This innovative development was made possible through advanced technologies and methods, including the use of big data and of spatial transcriptomics, a technique that reveals where genes are active in a tissue. "We mapped the spatial immune architecture in human tumors at single-cell resolution level and found that the TREM2-carrying macrophages were often positioned in direct proximity to immune killer cells that appeared exhausted," Xie says. "That spatial insight led us to design biological molecules that could block immune-suppressing macrophages while simultaneously delivering a localized activation signal to the killer cells, energizing them to attack the tumor while minimizing collateral damage."
This approach exemplifies a growing trend in cancer immunology: designing therapies that reshape the tumor microenvironment rather than focusing solely on killing cancer cells. "The future of immunotherapy lies in combining safety with precision - reprogramming the immune ecosystem from the inside rather than targeting cancer cells directly," says Amit.
In studies in mice, MiTEs caused tumors to shrink and triggered widespread immune remodeling in both macrophages and immune killer cells. When tested on tissue samples of renal cell carcinoma derived from patients, they caused robust immune activation, including the awakening of killer immune cells. To take MiTEs another step toward clinical application the scientists plan to assess their long-term safety and further explore combinations with existing therapies, including chemotherapy and radiation therapy. Preliminary results suggest that MiTEs act synergistically with existing checkpoint inhibitors, amplifying the overall immune response.
The findings provide a blueprint for a new generation of safe and programmable immunotherapies capable of overcoming resistance to current treatments in a wide spectrum of malignancies. "Our work demonstrates that by understanding the tumor's own defense mechanisms, we can turn them into opportunities," concludes Amit. "With MiTEs, we may have found a way to convert the tumor's shield into the very weapon that defeats it."

Science Numbers
To characterize the distribution of the TREM2 receptors and find the optimal enzymes to unmask the immune-activating molecules, the researchers mapped 13.8 million cells from 5,400 patients.
Also participating in the study were Dr. Diego Adhemar Jaitin, Dr. Fadi Sheban, Dr. Chamutal Gur, Reut Sharet Eshed, Eyal David, Kfir Mazuz, Dr. Roberto Avellino and Dr. Assaf Weiner from Amit's lab in Weizmann's Systems Immunology Department; and Dr. Adam Yalin, Dr. Florian Uhlitz, Caroline Jennings Marin, Dr. Ankita Sankar and Devin Mediratta from Immunai, New York, NY.
Prof. Ido Amit is the incumbent of the Eden and Steven Romick Professorial Chair.
Prof. Amit's research is supported by the Moross Integrated Cancer Center; the Elsie and Marvin Dekelboum Family Foundation; the Lotte and John Hecht Memorial Foundation; and Daniel Andreae.






