A new study suggests that lab-grown oral mucosa successfully can be used for testing biological effects of dental materials. The project is a collaboration between the Institute of Oral Biology (IOB) and the Nordic Institute of Dental Materials (NIOM) and is published in Biomaterial Investigations in Dentistry.
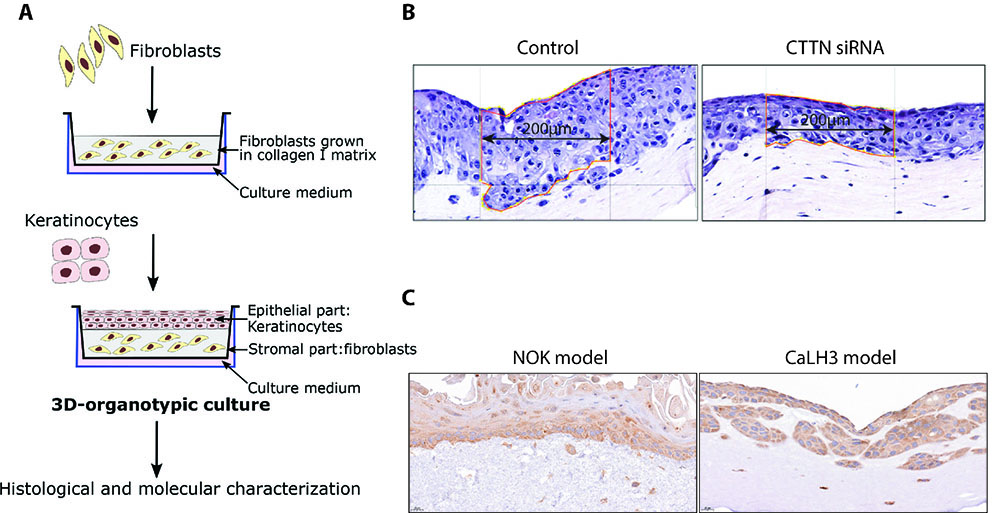
Figure 1: A) Schematic illustration showing construction of 3D model. B) Representative example of 3D models consisting of oral cancer cells showing reduction of epithelial thickness after siRNA mediated silencing of the CTTN gene in cancer cells. Epithelial thickness was calculated by dividing the area of the epithelium by its length (Figure adopted from Toközlü SB, Eur J Oral Sciences, 2023). C) 3D models of NOK (left) and oral cancer (CaLH3) cells (right) showing expression of p62, a marker for autophagic flux.
The oral cavity is continuously exposed to a range of chemical substances released from dental materials used in dental fillings and prostheses. Since these materials will be in the mouth for a longer period, it is important that dental materials are safe and do not cause adverse effects on structures in the oral cavity, including the oral mucosa. Therefore, investigation of biological effects of dental materials using suitable laboratory model systems is crucial in the development and/or refinement of dental materials. In this regard, single-cell cultures (epithelial cells, fibroblasts) derived from oral mucosa and grown as a two-dimensional (2D) culture have been widely used for this purpose.
3D models that mimic the structure of oral mucosa
As oral mucosa is a complex three-dimensional (3D) structure consisting of various cell types, using 2D model systems is inadequate to understand the cellular processes dependent on cell-cell interactions between different cell types and to obtain clinically relevant biological effects of dental materials. In this context, in vitro, 3D models consisting of different cell types are gaining popularity in life science research. We have successfully used 3D models consisting of normal oral keratinocytes (NOK) and cancerous keratinocytes grown on top of a collagen matrix consisting of normal oral fibroblasts (NOF), thereby mimicking normal oral and cancerous oral epithelium (Figure 1A). We have previously used these models to examine
- i) proliferation, differentiation, and invasion and of tumor cells (Sapkota D, BMC Cancer, 2015; Toközlü SB, Eur J Oral Sciences, 2023) (Figure 1B), and
- ii) interaction between bacteria and oral epithelium (Dabija-Wolter G, Arc Oral Biol, 2012).
Investigating the biological effects using 3D models
In the current study, a collaborative project between the Institute of Oral Biology (IOB) and the Nordic Institute of Dental Materials (NIOM) recently published in Biomaterial Investigations in Dentistry, we have investigated the biological effects of 2-hydroxethyl methacrylate (HEMA), a major constituent of dental resins, on laboratory engineered 3D-organotypic models of oral mucosa. The 3D models were created by co-culturing NOK on top of a collagen I matrix consisting of NOF. Using several analysis methods (morphometric/histological analysis, qRT-PCR, immunohistochemistry), the treatment of 3D models consisting of OEC and NOF was found to increase apoptosis of NOK. Besides, HEMA treatment was found to increase autophagy flux in NOK as indicated by the expression of SQSTM1 mRNA and corresponding protein levels (Figure 1C). These results indicate that 3D-organotypic co-cultures of NOK represent a biologically relevant model system for investigating the biological effects of HEMA and other dental biomaterials.
Nevertheless, establishing and maintaining NOK culture is expensive and difficult, as NOKs tend to differentiate after a limited number of passages in 2D cultures. Hence, we investigated the possible use of oral cancer cells as an alternative to NOK for 3D models. Our results indicated that 3D-co-cultures of NOK and oral cancer cells reacted similarly to HEMA treatment with respect to cell proliferation and activation of autophagy flux. These observations open the possibility for the use of 3D models based on oral cancer cells as an easier and cheaper model system for testing biological effects of dental materials.
These models are flexible with respect to the cell types, timepoint, and duration of treatment and offer a wide range of downstream analysis possibilities (morphometric/histological analysis, global and pathway-focused molecular analysis) using the artificial tissue or culture medium.
References
Dabija-Wolter G, Sapkota D, Cimpan MR, Neppelberg E, Bakken V, Costea DE. Limited in-depth invasion of Fusobacterium nucleatum into in vitro reconstructed human gingiva. Arch Oral Biol. 2012
Sapkota D, Bruland O, Parajuli H, Osman TA, Teh MT, Johannessen AC, Costea DE. S100A16 promotes differentiation and contributes to a less aggressive tumor phenotype in oral squamous cell carcinoma. BMC Cancer. 2015
Sharma S, Khan Q, Schreurs OJF, Sapkota D, Samuelsen JT. Investigation of biological effects of HEMA in 3D-organotypic co-culture models of normal and malignant oral keratinocytes. Biomater Investig Dent. 2023
Toközlü SB, D. Sapkota, E. M. Vallenari, O. Schreurs, T. M. Søland. Cortactin expression in a Norwegian cohort of human papillomavirus negative oral squamous cell carcinomas of the mobile tongue. Eur J Oral Sciences. 2023






