It was meant to be the last day of Debbie Menzies' life. Standing on the Golden Gate Bridge, she contemplated the last-but-one task on her agenda: Where to leave her keys and wallet.
And then she felt a tap on her shoulder, followed by a steady voice. "Are you OK?"
Years after that encounter with a bridge patrol officer, Debbie reframes that day as the "beginning of a brand new life." She didn't know it then, but now she can identify that as the moment that put her on a new path that would lift a burden that had weighed her down for nearly five decades.
It was in the early 1970s when Debbie, then 8, developed seizures and was diagnosed with epilepsy. She would feel an "electrical sensation" in her head, pick at her clothes, and dissolve into strange, unhappy laughter. Sometimes she was unable to talk for several seconds. Classmates would stare, then recoil, and gather into groups to snicker.
Her parents advised her "'not to air my dirty laundry,'" she says; "my seizures were my dirty laundry." They referred to the seizures as "spells," reinforcing their sinister connotation. Growing up in a suburb of Portland, Maine, Debbie felt ashamed, unworthy, and very much alone.
Anti-seizure medications were explored. Some worked partially; all had unpleasant side effects. Like many patients with epilepsy, Debbie had difficulty retaining information. In 1982, at 19, her fear of flunking her second year of college drove her to her first suicide attempt.
Sessions with a therapist helped her stabilize, and she experienced an extended period of relative calm. Eventually, she found work as a legal secretary, moved to California, married her longtime boyfriend, Robert, and had their son, Jeremiah.
But the seizures persisted. Years later, she learned they were called gelastic seizures, named after the ancient Greek word "gelos" for laughter. They occurred several times a day and were sometimes accompanied by atonic seizures, that made her fall or slump forward, and tonic-clonic seizures, causing writhing and convulsing. Feeling like she'd reached the end of the line, Debbie shared her intention to end her life and was hospitalized for a second time.
I wonder, sometimes, what my life would be like if I'd received this treatment earlier...
Debbie Menzies
Brain surgery in real-time, thanks to NIH funding
Depression descended on her again in 2018, following a stinging email from a lawyer at her workplace. This time, the Golden Gate Bridge beckoned.
Debbie doesn't recall her early days at Priscilla Chan and Mark Zuckerberg San Francisco General Hospital and Trauma Center (ZSFG), where she was hospitalized for weeks following her encounter with the bridge patrol officer. But she remembers meeting Paul Garcia , MD, a professor of neurology at UC San Francisco. The two institutions have a long history of collaboration, with UCSF physicians treating patients at ZSFG.
After hearing about Debbie's gelastic seizures, Garcia ordered a brain MRI that revealed the tiny tumor-like growth that he had predicted. That eureka moment prompted a diagnosis: hypothalamic hamartoma.
"Gelastic seizures are a hallmark of this disorder. Mood swings, depression, and anger, as well as problems with memory and attention are also symptoms," said Garcia. "That's because the location of the growth, the hypothalamus, is a critical component of the limbic system, the brain structures that control emotions and memory."
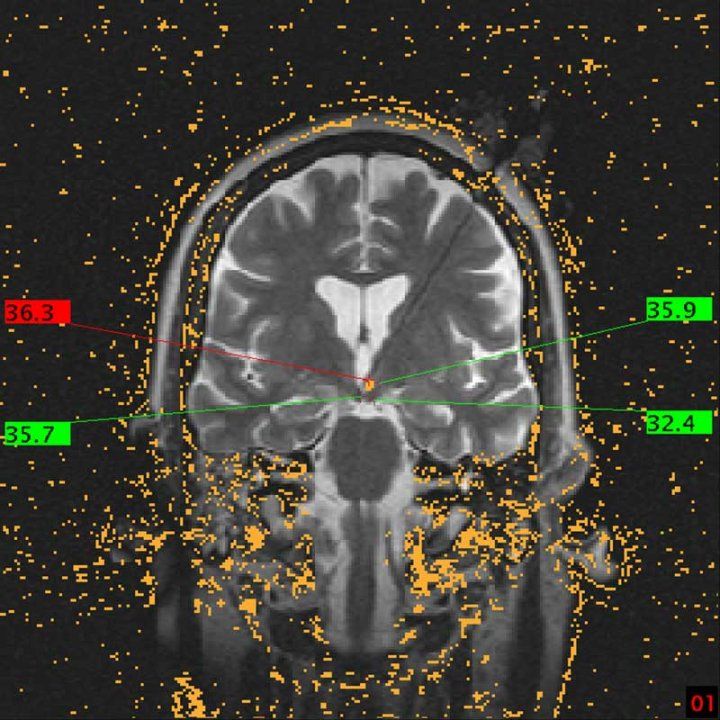
Hypothalamic hamartoma used to be removed via open brain surgery, a risky procedure due to its proximity to vital structures. Renown neurosurgeon Edward Chang , MD, agreed to treat Debbie using a procedure known as laser interstitial thermal therapy (LITT). The technology had been refined at UCSF with the aid of a National Institutes of Health (NIH)-funded MRI suite that allows a neurosurgeon to see the growth in real time and avoid adjacent areas responsible for memory, vision, and hormone function.
While Debbie was under anesthesia, Chang inserted a laser-tipped probe through a small hole in the skull deep within the middle of her brain. Once positioned, the laser converted to thermal energy that precisely heated and destroyed the growth. This technique results in a faster recovery and significantly reduces the risk of complications.
Since that surgery, more than six years ago, Debbie says she has not had a single seizure nor suffered with depression. While she experiences the full spectrum of emotions, she no longer finds that negative ones accelerate to desperation.
"I wonder, sometimes, what my life would be like if I'd received this treatment earlier," she says. "But mainly, I worry about other people with the same symptoms. Certainly, there are others out there with hypothalamic hamartoma. They are going through what I went through because they haven't received the correct diagnosis and treatment."

If you are having thoughts of suicide, call or text 988 to reach the 988 Suicide and Crisis Lifeline. SpeakingOfSuicide.com/resources lists additional resources.






