
Epilepsy affects one in every 100 people-1 million in Japan and 50 million worldwide. It is the third most common brain disease after stroke and dementia. In Japan, its incidence and prevalence have been increasing among the rapidly aging population. Prof. MATSUMOTO Riki of Kobe University Graduate School of Medicine is fascinated by the complexities of the human brain, and he specializes in the research and treatment of epilepsy. Twenty years ago, he discovered a new mapping method for human brain connectivity.This method has been used clinically in many parts of the world because of its usefulness in diagnosing and surgically treating brain disorders. Prof. Matsumoto contributed to the inauguration of the first Hyogo Prefecture-designated regional epilepsy center in May 2022. His life revolves around improving the well-being and quality of life of patients with epilepsy. We interviewed him to learn about the basics of epilepsy and his recent activities.
Brain Microcosms
What motivated you to become a neurologist?
Professor Matsumoto: When I was in the 11th or 12th grade of high school and contemplating my future career, I had two options: to be a space engineer or a physician. My father was a faculty member who specialized in space engineering. Although the idea of launching space rockets was exciting, I chose to study medicine. I had a brother with perinatal cerebral palsy and I wanted to explore the mechanisms behind how brain injuries prevent people from walking or speaking. The brain is the center of the body's entire nervous system including the spinal cord and peripheral nerves innervating the internal organs and the muscles in the extremities. It contains tens of billions of neurons, creating a network with a microcosmic, complex architecture. I was attracted by these magnificent yet enigmatic aspects of the human brain.
We are told that the brain's functions largely remain unknown. How much do we actually know?
Prof. Matsumoto: The brain is like a "black box." Brain science is an uncharted territory, yet an increasing body of knowledge has developed regarding the speech, auditory, and motor functions of the brain. Yet, we are very far from completely understanding them. Little has been discovered about the complex prefrontal mechanisms that regulate thought, intelligence, and emotion. My motivation for clinical research is to understand the mechanisms, functions, and dysfunctions of the brain scientifically and to thereby provide therapeutic interventions.
You specialize in epilepsy care. Could you tell us what prompted you to do so?
Prof. Matsumoto: Neurology covers many types of neurological disorders other than epilepsy. Typical examples include stroke and dementia, which often develop in elderly people. Neurology also addresses intractable neurological conditions such as Parkinson's disease and amyotrophic lateral sclerosis. Neurologists provide pharmaceutical and other non-surgical options for treatment, whereas neurosurgeons surgically treat the conditions. During my residency at the Department of Neurology, I chose to specialize in epilepsy because it is now a controllable disease, thanks to the many available treatment options that range from pharmacotherapy to surgery. I thought that treating patients with epilepsy would be a rewarding experience for me.
The neuronal activities in the brain generate electrical pulses, which can be recorded using electroencephalography (EEG). Patients with epilepsy develop seizures as a result of abnormal electrical activity that occurs in an otherwise normally functioning brain. If you understand the functions of brain systems, you can understand how epileptic seizures occur. It is the normally functioning brain systems that produce epileptic seizures when the system is involved in abnormal electrical activities. In this sense, epilepsy is a disease attractive for neurologists who have interest in understanding how the brain is wired and making use of this knowledge to treat the disease.
Please enlighten us about the symptoms and treatment of epilepsy.
Prof. Matsumoto: Depending on the affected region, epileptic seizures can be divided into two major categories: generalized and focal. Generalized seizures refer to the condition in which the entire brain is affected. Generalized seizures cause the whole body to shake or stiffen. Focal seizures originate from a specific part of the brain, and their symptoms are related to the functions of the affected area. Typical symptoms include involuntary limb movements, unresponsiveness and impaired consciousness. Patients with focal seizures may experience sudden twitching or jerking of the arm that cause them to drop the things they are holding. Approximately 70% of patients with epilepsy can be managed with drugs, but the rest are refractory to pharmacotherapy. When the epileptic focus is well identified by detailed examinations such as EEG recording of seizures and magnetic resonance imaging (MRI), epilepsy surgery, namely, surgical removal of the epileptic focus while preserving other brain areas is an option for patients with refractory epilepsy to cure the disease.
Leading the Epilepsy Center
The Epilepsy Center was recently established at Kobe University Hospital, and you serve as the founding director. What role does the center have?
Prof. Matsumoto: Epilepsy is the third most common neurological disorder after stroke and dementia. Its onset usually occurs at an early age. However, the rapid aging of the Japanese population has increased the number of elderly patients who experience seizures after stroke, dementia, or traumatic brain injuries. Against this backdrop, in 2018 the Ministry of Health, Labor, and Welfare started a national initiative to establish a network of regional hub centers for epilepsy treatment. Through this program, each prefectural government is encouraged to designate a hub center within its jurisdiction. In cooperation with the Hyogo branch of the Japan Epilepsy Association, a leading patient advocacy organization, we worked with the Hyogo Prefectural Government to establish the Epilepsy Center in May 2022.
Treatment and care of patients with epilepsy require a multidisciplinary approach involving pediatricians, neurologists, psychiatrists, neurosurgeons, and many more. Since my appointment as professor at Kobe University in 2018, I have been hosting interdisciplinary case conferences once a month. Since 2021, Kobe University Hospital has been providing surgical services for patients with drug-refractory epilepsy. At our hospital, more than 50 patients undergo long-term video-EEG monitoring annually, which is a technique to evaluate epileptic brain activity for accurate diagnosis and surgical approach. In November 2022, we opened a medical call center for patients with epilepsy, where various specialist physicians provide consultations three times a week. In addition to providing medical care, we are going to help patients retain their independence by supporting them through significant life events such as school admission, employment, and marriage.
In your research and treatment of patients with epilepsy, you have discovered a new brain wave monitoring technique that is of great help to diagnosis and surgical treatment.
Prof. Matsumoto: I had a two-year clinical fellowship from 2000 to 2002 at the Cleveland Clinic in Ohio in the United States, one of the world's leading epilepsy surgery centers. During that time, I discovered what is termed the "cortico-cortical evoked potential" (CCEP) mapping technique, which was published in 2004.
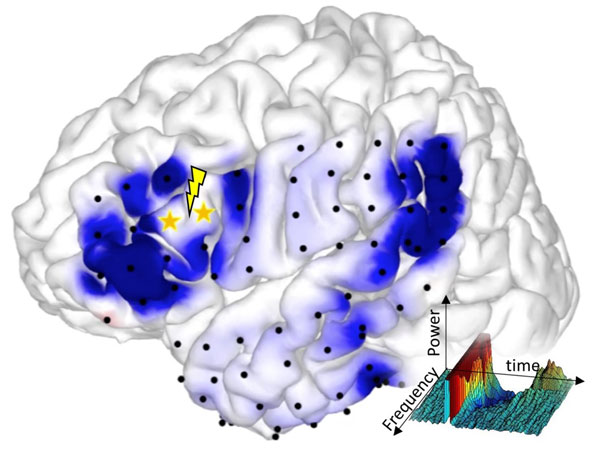
The human brain's higher functions such as language processing are maintained by the neural networks that connect different regions of the cerebral cortex. During epileptic seizures, these neural networks become overactivated and transmit excessive electrical signals to generate seizure attacks. Recent advances in MRI techniques have enabled us to visualize large fiber bundles in the white matter. However, MRI does not allow us to trace the fiber bundles into the cerebral cortex, or to know how cortical neurons are interconnected.
My colleagues and I found that when weak single-pulse electrical stimuli are applied to a particular region of the cortex at a frequency of 1 Hz (one cycle per second), CCEPs are recorded at functionally connected sites. Electrical signal is conveyed via the axons (fibers) of cortical neurons to reach the target cortex and generate brain evoked potentials, namely, CCEPs. This method is useful for identifying cortico-cortical connectivity. For example, Broca's and Wernicke's areas represent the regions of the brain that are responsible for language processing. These two areas are connected by a large fiber bundle, the arcuate fasciculus. Therefore, when Broca's area is electrically stimulated, CCEPs are detected in Wernicke's area. In this way, we can identify the brain network important for language processing for patients undergoing brain surgery.
In the surgical treatment of brain tumors located in proximity to the cortical and subcortical language fibers, CCEP monitoring helps preserve them. This technique has been employed in brain tumor and epilepsy surgery across the globe. Given that epilepsy is a disorder of pathological excitation/dysfunction of the neural network, the CCEP monitoring technique is also useful in identifying the epileptic foci and network.
Minimally Invasive Approach to Developing the Functional Brain Map
You are the principal investigator of a project recently approved under the Kobe University Strategic International Collaborative Research Grant* (FY2022-2024). Entitled "Development of a global-standard, minimally invasive functional brain network mapping technique for brain surgery," this project aims to expand the utility of the CCEP monitoring technique. What are the specific objectives and expected results of the project?

Prof. Matsumoto: In collaboration with Prof. Duffau of University of Montpellier, France, this project aims to develop a minimally invasive method for creating functional brain maps using electrical stimulation. The white matter underlying the cerebral cortex is largely composed of fibers (axons) originating from neurons. The functions of the white matter remained largely unknown until the 21st century. Prof. Duffau was among the first to determine the function of the white matter fiber bundles by applying high-frequency electrical stimuli during brain surgery. Prof. Duffau and I were interested in optimally preserving healthy brain tissue during surgical treatment of brain tumors and epilepsy. He asked me to start the collaboration in 2021. This project will develop a transdisciplinary methodology with the help of Dr. Bonnetblanc, a bioinformatics expert and senior researcher at the French National Research Institute for Informatics and Automatics (INRIA).
The focus of this project is to develop a minimally invasive approach for brain mapping, which means keeping electrical stimuli as weak as possible. Applying strong electrical current in the vicinity of epileptic foci may trigger the epileptic seizures. There has been no reported human brain connectivity map that spans the cortical and subcortical neural networks using the gold-standard mapping method of electrical stimulation-we aim to establish the first of its kind for clinical brain mapping.
Resume
| March 1994 | Graduated from the Faculty of Medicine, Kyoto University |
|---|---|
| April 1998 | Started the doctoral program at Kyoto University Graduate School of Medicine |
| July 2000 | Started clinical fellowship at the Section of Epilepsy and Clinical Neurophysiology, Department of Neurology, Cleveland Clinic |
| March 2003 | Obtained MD-PhD degree |
| April 2007 | Appointed Assistant Professor, Department of Neurology, Kyoto University Hospital |
| August 2016 | Promoted to Associate Professor, Department of Neurology, Kyoto University Graduate School of Medicine |
| December 2018 | Elected Professor and Chair, Division of Neurology, Kobe University Graduate School of Medicine |
| February 2021 | Concurrently appointed Director Assistant, Kobe University Hospital |
| April 2021 | Concurrently appointed Director of the Center for Cognitive and Memory Disorders, Kobe University Hospital |
| May 2021 | Also appointed Director of the Epilepsy Center, Kobe University Hospital |
*Note
Professor Matsumoto's project has been approved as a Type B project under the Kobe University Strategic International Collaborative Research Grant program.
- Kobe University's research highlights:






