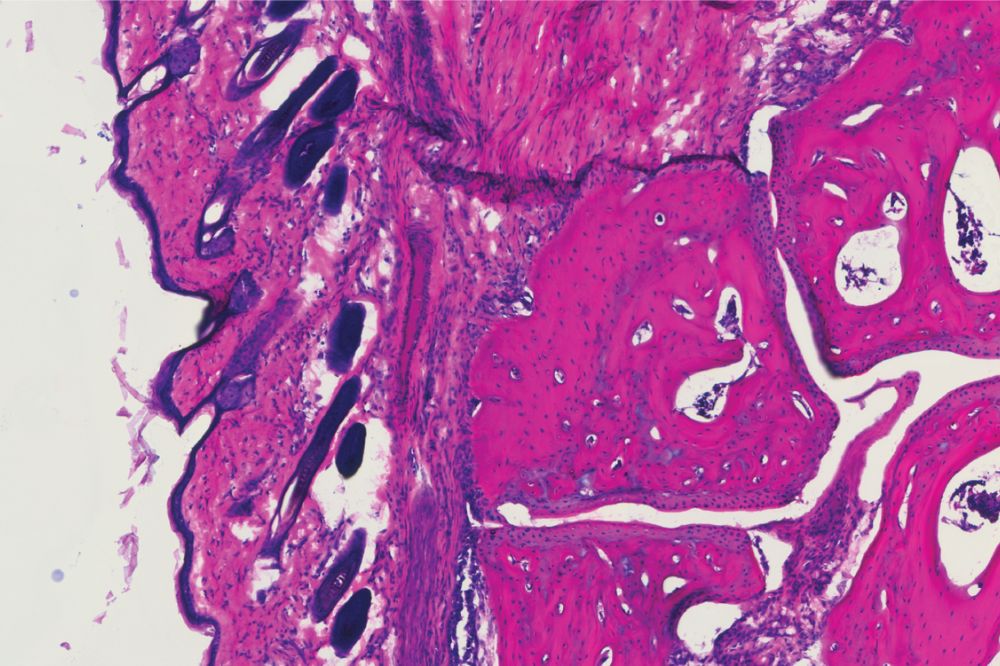
A histology showing the ankle joint of a mouse four days after receiving the new antibody treatment, V11 sFc (Ravetch lab)
Intravenous immunoglobulin (IVIG) therapy involves infusing patients with naturally occurring IgG antibodies to treat autoimmune conditions. With origins dating back to the 1950s, IVIG is currently FDA-approved for four diseases but widely prescribed off-label to treat more than 80 additional ones because it's often the only medicine that has any impact on these conditions.
But IVIG has serious shortcomings. Treatment can require multi-hour, high-volume infusions several times per month, the cost is exorbitant, and because the antibodies are sourced from donated human plasma, there are frequent supply shortages.
Now scientists from Rockefeller University's Leonard Wagner Laboratory of Molecular Genetics and Immunology have used their discovery of previously unknown mechanisms in an anti-inflammatory pathway to develop a powerful upgrade: an engineered antibody that delivers the effectiveness of IVIG at fraction of the dose in mice, and can be synthesized without the need for human plasma. They published their results in Science.
"We discovered that by enhancing the binding of a certain pair of receptors we can significantly lower the dose yet have an equal effect," says first author Andrew Jones, a research associate in the lab, which is led by Jeffrey Ravetch.
These advances build upon earlier research from the lab that have already led them to develop a molecule 10 times more potent than IVIG, which is currently in phase 2 clinical trials through the biotech company Nuvig that Ravetch co-founded. The current findings dramatically improve upon that molecule.
40 years of research
The findings build on 40 years of research in Ravetch's lab on Fc receptors, a family of proteins found on the surface of nearly all immune cells to which antibodies bind to coordinate the immune system's effector responses. The most common serum antibody is immunoglobulin G (IgG), which represents 75% of the infection-fighting force found in blood-and is the key component of IVIG.
The work on the anti-inflammatory properties of IVIG began about 25 years ago when Ravetch discovered that a small fraction of serum IgGs present in IVIG possessed a naturally occurring modification: a sugar modification called sialylation, which conferred its anti-inflammatory properties. Subsequent studies in his lab identified two additional components that were required to trigger an anti-inflammatory response by IVIG: an inhibitory Fc receptor called FcγRIIB and a lectin (a carbohydrate-binding protein) called DC-SIGN. These insights led them to be able to develop the drug currently in phase 2 clinical trials, now known as NVG-2089, which is 10 times more potent than IVIG in suppressing autoimmune inflammation.
"Those were the pieces that we had figured out," Ravetch says. "The question was, how do these three components come together to mediate the anti-inflammatory activity? That's the work we undertook for the current study."
That earlier work had also been done studying IVIG activity in mice with their own native Fc receptors-not human ones. Since then, Ravetch has developed mice that express human Fc receptors.
"We thought we could potentially develop a next-generation therapeutic IVIG if we had a better understanding of how IVIG works specifically on cells expressing human Fc receptors," Jones says.
Powering up
To understand how these components come together to mediate IVIG activity, the researchers conducted many in vitro experiments testing a variety of scenarios of activation and interaction.
"We discovered that the type 1 FcγRIIB receptor and the type 2 DC-SIGN co-receptor are actually binding to each other on the cell surface, and that seems to be important for the anti-inflammatory effect of IgG," Jones says. "This was a novel configuration we hadn't seen before. We think that when they bind, they enhance the ability of the sialylated IgG antibody to trigger the anti-inflammatory signaling cascade."
They next engineered a recombinantly expressed IgG to have enhanced binding to these receptors and infused them into mice with human Fc receptors into which they had induced arthritis (meaning they'd been injected with serum isolated from a mouse with naturally occurring arthritis). A similar group of arthritic mice was treated with the conventional IVIG infusion.
Both groups benefited from the infusion, seeing reduced joint swelling. But the doses were dramatically different: 100 times as much IVIG was required to achieve the same effect as one dose of the new molecule.
"This is a really substantial difference, and there are several factors why it's important. For one, this new molecule is a recombinant protein that we can produce in vitro, so it does not need to come from human plasma. That's an enormous advantage," Ravetch says. "And then there are the many autoimmune diseases that currently aren't treated with IVIG because we haven't achieved the correct dosing. With a very high potency product, it's possible to achieve the correct dosage and expand use to more autoimmune diseases."
A second test run used a mouse model stand-in for multiple sclerosis, an autoimmune disease that causes both cognitive and mobility deterioration. The molecule protected mice from neuro-inflammation by preventing cell destruction, and did so at the same small dose.
Going forward, the lab will look into the structure and molecular dynamics of the type 1 and type 2 receptors. They've identified many over the years, but how they pair up and what their functions are remain to be discovered. "What we have discovered opens the door to exploring how they might function in different biological pathways," Jones says.
They'll also pursue clinical potential. "As of now, we've optioned the molecule to Nuvig, and they'll test further to determine if they want to pursue it as a clinical product," Ravetch says. "I hope they do. We want to see it get into patients."






