30 Years Ago, Scientists led by Nancy Wexler Identified Cause of the Disease
By Sharon Tregaskis
Ai Yamamoto was a Columbia PhD student deep in the throes of writing her dissertation on an inducible mouse model of Huntington's disease when she found a box of truffles on her desk. Flown in from Switzerland just hours earlier, these were no common chocolates. "Your work is important," read the accompanying note.
"I was a grad student and if it had been a free bag of M&Ms, I would have been touched," says Dr. Yamamoto'01 PhD, now associate professor of neurology and pathology & cell biology at VP&S. That the confections were an extravagant and coveted indulgence made the gift even more meaningful-especially considering the source.
The encouraging note was signed by Nancy Wexler, PhD, the Higgins Professor of Neuropsychology in Psychiatry, Neurology, and Neuroscience at VP&S; president of the Hereditary Disease Foundation (HDF), an organization helping to fund Dr. Yamamoto's graduate studies; and an acknowledged leader of basic and applied research in Huntington's disease. And Dr. Wexler was right about the importance of Dr. Yamamoto's work: The younger scientist's dissertation project-published, in part, by the journal Cell in 2000- demonstrated that Huntington's disease can be reversed in a mouse model of the fatal, neurodegenerative, genetic illness characterized by involuntary movements and cognitive and psychological changes.
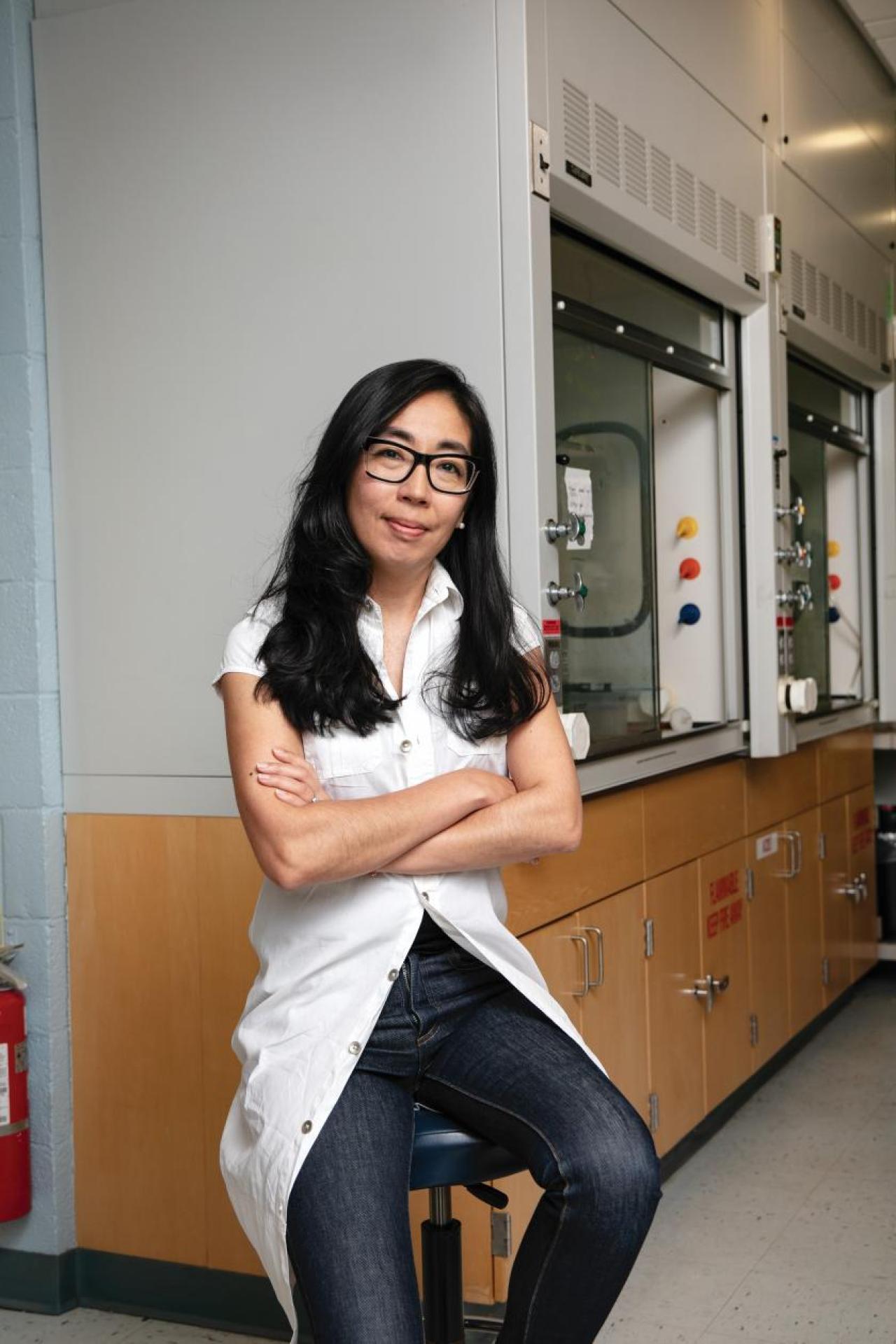
Ai Yamamoto. Photo by Jorg Meyer.
Two decades later, Huntington's remains a core focus of Dr. Yamamoto's NIH-funded efforts to understand the housekeeping processes used by cells within the brain to preserve homeostasis, work that has implications for cardiovascular disease, obesity, and a host of neurodegenerative disorders. Dr. Yamamoto is an advisory board member for both the Hereditary Disease Foundation and Project ALS.
Team Science
In 1980, funded partly by the Hereditary Disease Foundation, geneticist David Housman, now the Ludwig Professor of Biology at the Massachusetts Institute of Technology, and his former student James Gusella, who is the Bullard Professor of Neurogenetics at Harvard Medical School, launched a quest for the gene that causes Huntington's disease. Forty years ago this year, these scientists, along with Dr. Wexler and several others, found a clue to its location, a marker on the upper arm of chromosome 4. Their reverse genetic screen also provided proof of concept for the groundbreaking Human Genome Project, while the scientists' dynamic partnership with affected families became a model for rare disease research and advocacy.
The key to that partnership-and to finding the gene-was Dr. Wexler, who in 1981 began her annual month-long trips to Venezuela to study and bring aid to the families with Huntington's living around the shores of Lake Maracaibo, the largest known cluster of such families anywhere in the world. The enormous pedigree she and her team created, the blood and skin samples they collected, and neurological tests they administered and recorded provided the essential data that made possible the discovery of the genetic marker and eventually the Huntington's gene. Dr. Wexler's team called itself the US-Venezuela Huntington's Disease Collaborative Research Group: clinicians and scientists whose experience in Venezuela-for some of them year after year for over two decades-helped them become leading international experts on Huntington's and the mentors of several generations of clinicians.
Dr. Housman credits Dr. Wexler with championing a principle that has guided him over nearly five decades in the classroom and in his own research. "You have to know the patients and their families and you have to know them as well as you possibly can, because the information that they hold is what will allow you to understand the disease and its consequences and its behavior," he says. "That approach was brought to the science table by Nancy."

GENE HUNTERS: Huntington's Disease Collaborative Research Group and Advisory Committee meeting in Florida, circa 1989. Photo courtesy of Hereditary Disease Foundation.
Soon after the 1983 marker discovery, Dr. Wexler, Dr. Housman, Dr. Gusella, and other "gene hunters" established what they called the Huntington's Disease Collaborative Research Group. They vowed to share materials and insights as they traveled the distance from the marker to the gene. Along the way they invented a host of technologies since deployed in work on hereditary heart diseases, Alzheimer's, and ALS. Then in March 1993, they found the gene itself: IT15. Published in the journal Cell, the report identifying IT15 was coauthored by the Huntington's Disease Collaborative Research Group, an unusual collective authorship at the time that was testament to the power and synergy possible through team science. "The challenge is best met by having people work together," says Dr. Housman. "In science, that's the best way to get things done." For her role in the discovery, Dr. Wexler was awarded the 1993 Mary Woodard Lasker Public Service Award.
Dr. Housman, who has continued publishing with Dr. Wexler on Huntington's throughout the intervening decades, credits her with humanizing clinical and basic research not only in Huntington's, but also in a host of rare diseases. "Every single Hereditary Disease Foundation workshop started with a meeting with someone with Huntington's disease and often with someone with Huntington's and their family," he says. "As I started to teach medical genetics in the Harvard-MIT program, that's what we incorporated into our course."
Basic Biology
Every human being has two copies of IT15-one from each parent. In an inheritance pattern known as autosomal dominant transmission, it takes just one unstable form of IT15, from either parent, to induce symptoms of Huntington's. Over the past three decades, hundreds of scientists have pitched in to elucidate the effects of IT15, which features a repeat of the trinucleotide sequence cytosine-adenine-guanine, or CAG, and encodes for a huge protein known as huntingtin.
Most of us inherit a form of IT15 that has fewer than 27 CAG repeats. The resulting huntingtin serves as a scaffolding protein imperative for embryonic development and implicated in a host of normal cellular functions. We can't live without it. Among people with Huntington's-approximately 3 of every 100,000 people worldwide-gene instability multiplies the CAG repeats, resulting in a bulky and fragile form of huntingtin that shatters and aggregates in sticky clumps within the deep-brain region known as the striatum. Cognitive and psychiatric symptoms-forgetfulness, apathy, irritability, depression-often precede motor symptoms that include stumbling, slurred speech, and kinetic, uncontrolled movement. While there is no treatment yet for humans to prevent, slow, or reverse the progression of the disease, medications can calm movements and relieve depression and irritability.
As a grad student fueled by Swiss chocolates, Dr. Yamamoto engineered mice in which the mutant gene identified by the Huntington's Disease Collaborative Research Group could be turned on and off with a dose of antibiotic. When she activated the gene, the mice developed movement disorders. Necropsy showed that clumps of huntingtin clogged their brains. Among the mice in which she turned off the gene after they began exhibiting movement disorders, the symptoms disappeared. So, too, did the cellular debris. "People talked about curing neurodegenerative disease, but it was theoretical," says Dr. Yama- moto. "I was as stunned as everyone else that the aggregates cleared."
Huntington's is not the only neurodegenerative disease characterized by protein aggregates. Aggregates also form in the brains of people with Alzheimer's, ALS, and Parkinson's. As she investigated where the aggregates had gone in her inducible Huntington's mice, Dr. Yamamoto zeroed in on selective autophagy, the process cells use to seek, label, and ultimately recycle unwanted materials. "Huntington's is the springboard for my lab," she says. "As new questions arise in other disorders, we go back to Huntington's first to try to get a sense of what's going on and from there dive into diseases that are far more difficult to model in a mouse."
Family Matters
Dr. Wexler was just 23 years old and not yet a scientist when she resolved to dedicate her career to finding a cure for Huntington's disease. It was 1968 and her mother, Leonore Sabin Wexler, a former high school biology teacher who had earned a master's degree in genetics in Columbia's zoology program in the 1930s, had just been diagnosed with the progressive, neurodegenerative disease. Huntington's had slowly robbed Leonore's father and all three of her older brothers of their independence, starting when they were in their 40s, and eventually their lives. With Leonore's diagnosis came the knowledge that Nancy and her sister, Alice, each stood a 50-50 chance of also developing the disease, which typically becomes symptomatic in midlife. That same year Milton Wexler-Nancy's and Alice's psychoanalyst father who was also a graduate of Columbia with a PhD in psychology from Teachers College-launched the Hereditary Disease Foundation to support research toward a cure. Nancy earned a PhD in clinical psychology, joined the HDF's Scientific Advisory Board and board of trustees, and in 1981 (following an exploratory trip in 1979) began her annual research expeditions to Venezuela.
Between 1981 and 2002, researchers amassed 4,000 DNA samples and a genetic pedigree of over 18,000 people (with and without Huntington's), stretching back more than 10 generations over two centuries.
The first comprehensive clinical description of Huntington's was reported by George Huntington, a third-generation Long Island physician whose forebears had long treated an extended family afflicted with what was locally known as St. Vitus' dance, the name more commonly given to a transient form of chorea seen in children. In 1872, just one year after his graduation from Columbia's medical school, Dr. Huntington published "On Chorea," an overview of what are now known to be several distinct types of involuntary movement disorders, including the childhood form and, most significantly, the hereditary, degenerative form that would later become known as Huntington's chorea and, ultimately, Huntington's disease.
In addition to describing the vigorous, uncontrolled movement characteristic of all choreas, Dr. Huntington highlighted the cognitive decline and mood disorders common in the hereditary, adult-onset form. Disease progression was relentless and irreversible, noted Dr. Huntington, and "spoken of by those in whose veins the seeds of the disease are known to exist, with a kind of horror, and not at all alluded to except through dire necessity, when it is mentioned as 'that disorder.'"
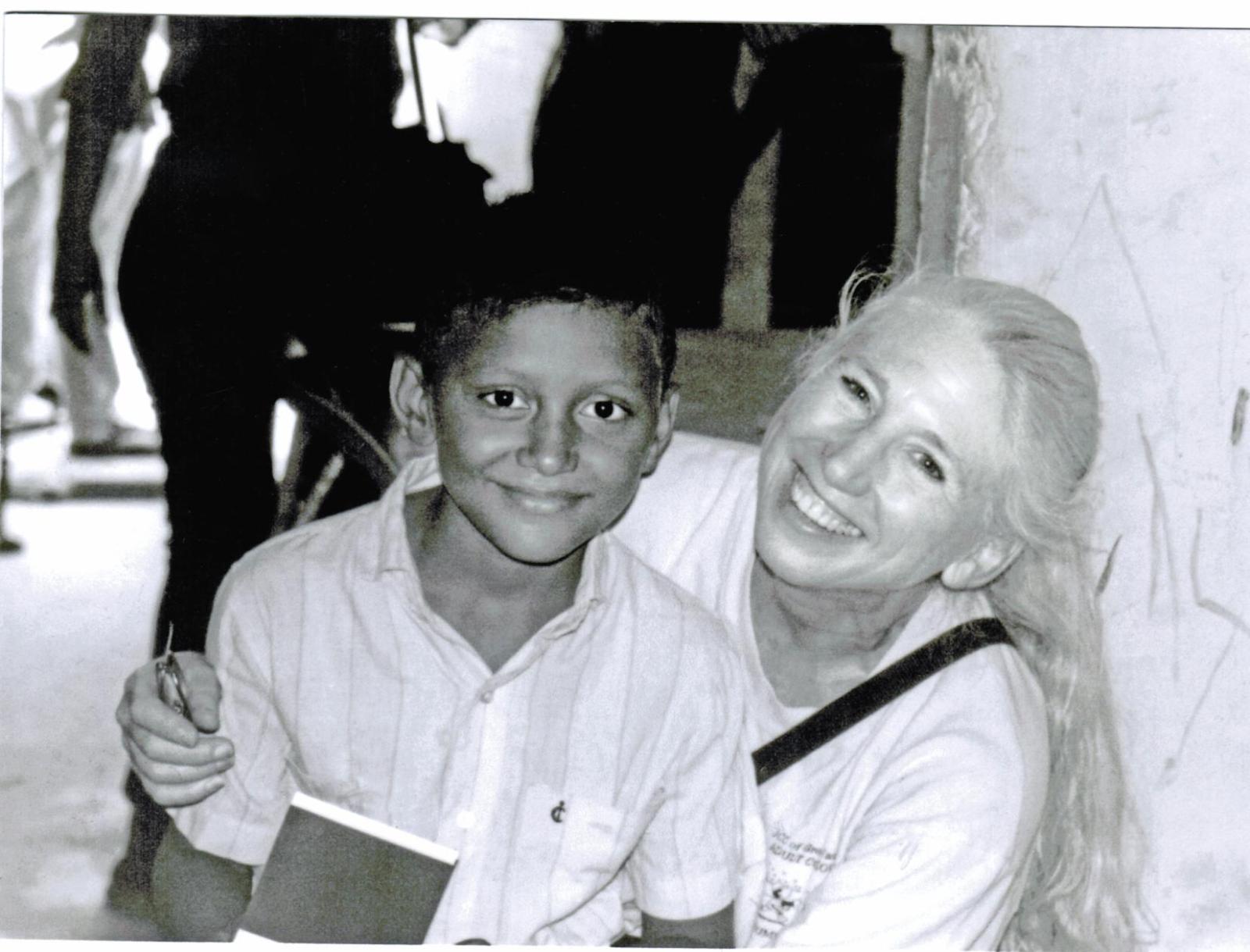
Nancy Wexler in Venezuela
As with the Long Island families, the much larger Venezuelan kindreds had themselves become experts in their disease. They understood its hereditary patterns and its physiological consequences exacerbated by stigma that had made them social outcasts and impoverished their families. They were skeptical when Dr. Wexler and other scientists, including Dr. Anne Young, today the Juliane Dorn Distinguished Professor of Neurology at Harvard Medical School, first arrived in their barrios and fishing villages, armed with vials and scalpels seeking to collect blood and skin samples. Dr. Wexler's Spanish was too rudimentary to explain that her own mother had had Huntington's and that she hoped through their participation to find the cause and eventually a cure for their affliction. An Argentinian nurse on the team broke through the language barrier, pointing out the scar on Dr. Wexler's arm from her own skin biopsy.
Between 1981 and 2002, the U.S.-Venezuela Huntington's Disease Collaborative Research Group would amass 4,000 DNA samples and a genetic pedigree of over 18,000 people (with and without Huntington's), stretching back more than 10 generations over two centuries. They performed hundreds of annual cognitive and neurological assessments. That body of data would prove vital to the 1983 gene marker discovery, the 1993 gene identification, the presymptomatic genetic test now widely available to people at risk of Huntington's, and insights into genetic and environmental modifiers of disease severity and age of onset. The work also led directly to the array of animal models now available to study the disease.
In recognition of the kindred's contributions, Dr. Wexler and her colleagues helped establish a nursing home and clinic in one of the barrios where many families lived. The Casa Hogar Amor y Fe was staffed by a Venezuelan doctor and by community members whose relatives had Huntington's. They provided tailored medical care until both home and clinic were closed by the Venezuelan government.
Clinical Questions
Neurologist Karen Marder, MD, founding director of Columbia's Huntington's Disease Society of America Center of Excellence, first met Dr. Wexler during her neurology fellowship at Columbia in the late 1980s. She joined Dr. Wexler on nine trips to Venezuela and helped develop the clinical rating scales of disease severity and progression still in use worldwide. Now the Sally Kerlin Professor of Neurology (in the Gertrude H. Sergievsky Center, in the Taub Institute for Research on Alzheimer's Disease and the Aging Brain, and in the Department of Psychiatry), Dr. Marder credits Dr. Wexler with bringing hope to the field. "Nancy is one of the most determined people I've ever met," says Dr. Marder. "She's taught a generation of neurologists and psychiatrists who wanted to take care of people with Huntington's a lot about how to make a difference."

Karen Marder. Photo by Jorg Meyer.
Even as the search for a cure continues, Dr. Marder and her colleagues focus on helping their patients live more comfortably and extend their quality of life through occupational, physical, and speech therapy; exercise; dietary modifications; and medications to treat neurological and psychiatric symptoms. Patients have opportunities to participate in a wide range of research trials, from observational studies seeking clues to the earliest signs of disease to clinical trials for emerging treatments.
The center also offers a robust, multidisciplinary approach to presymptomatic genetic testing. And while the stigma of Huntington's has shifted over time, due in no small part to the work of the Wexler family, getting a positive genetic test before the appearance of any symptoms continues to have profound psychological and social implications. The center requires psychiatric and neurological assessments and consultations with a genetic counselor and a social worker before testing to make sure that before being tested, people understand the deep implications and possible risks of choosing to learn such momentous information.
Huntington's was once considered evidence of the devil's touch, says Dr. Yamamoto. "Nancy brought it out in the open and got scientists working on it. Today, it's talked about in the same breath as Alzheimer's and Parkinson's, even though a lot fewer people have it. That's Nancy."
"We always ask each patient what they want to know from us," says social worker Deborah Thorne, who has worked at the center for three decades. While some people-an estimated 12%-17% of those at risk in North America and Europe-find presymptomatic genetic testing helpful to inform family planning or other long-range decision making, others-the vast majority-choose not to test, preferring to live with ambiguity and to make life plans on the basis of their 50-50 risk status (or, in some cases, opting for prenatal or preimplantation genetic testing when accessible).
For decades, in nearly every media interview about her work, Dr. Wexler fielded questions from reporters about whether she would be tested for Huntington's. She always demurred, highlighting instead the deeply personal nature of the decision. Then, in March 2020, at the age of 74, Dr. Wexler revealed in a New York Times interview that like her mother and grandfather before, she had Huntington's. "Having a fatal disease is scary and I don't want to trivialize that," she told the newspaper. "But if I can say 'I'm not stopping my life, I'm going to work, we're still trying to find a cure' that would help. If I can do anything to take the onus off having this thing, I want to do it."






