
As the world grappled with a pandemic, the lives of Patrick and Allison, empty-nesters living in Fresno, were hit by a series of extraordinary odds-defying occurrences.
The cause of that crushing fatigue Patrick experienced, just as they were about to reschedule the trip to Ireland that had been canceled due to COVID, was found to be a rare and deadly lung disease. The couple had pressed on. But their 30th wedding anniversary was spent on a siren-blaring, heart-thumping ambulance ride to their local hospital. After he was transferred to UC San Francisco, awaiting lung transplant, Patrick found out that he would be patient No. 1,000.
On April 13, 2022, the self-employed life-insurance agent, age 60, became the recipient of healthy transplanted lungs. "I don't like to use the word 'miracle' because not every patient gets that miracle, but I have received a new lease of life and I feel great.
Transplanted patients at UCSF, like Patrick, can live a normal life, with medications to ward off infections, healthy diet and exercise.
"I've had a good life - great family, great friends - and now I'm discovering I get to have more of the good life I've had before," said Patrick, who has leaned on his faith increasingly during his illness, as well as the prayers of more than 1,000 friends, family members and well-wishers.
In 2001, three-year survival for UCSF patients who had undergone lung transplantation was 50 percent. In 2021, it had reached 90 percent. And over the last 20 years, median survival has climbed from 3.5 years to 11.5 years.
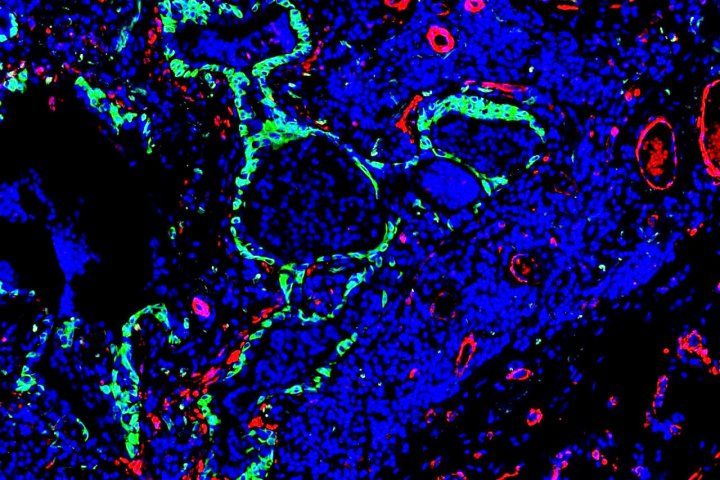
Innovations that have improved survival include the use during surgery of a type of life support, in which a machine pumps and oxygenates blood outside the body. Used in place of full cardiopulmonary bypass, it results in less bleeding and lung injury, and significantly reduces the risk of surgical airway complications, said Patrick's surgeon Jasleen Kukreja, MD, program and surgical director of the UCSF Lung Transplant Program.

Anti-rejection drugs and close patient surveillance, both in the days following surgery and the post-discharge period, have also contributed to excellent long-term outcomes, she said.
A program initiated by Kukreja, a few years ago, has improved access to donor lungs. The so-called ex-vivo lung perfusion process allows the lungs to be kept "alive" outside of the body in an environment that mimics the human body, while they are assessed for transplant suitability for a period of up to several hours.
"As a result of this program, we have transplanted several patients who otherwise would have had a 1 percent chance of receiving a match," she said.
Subtle Symptoms Foreshadowed Deadly Disease
For Patrick, the father of three twentysomethings who also live in Fresno, his illness started with subtle symptoms. "I had some shortness of breath when climbing up a hill, a couple of years ago. I simply figured I was too sedentary," he recalled. In May 2021, idiopathic pulmonary fibrosis was suspected by his pulmonologist, Kathryn Bilello, MD, of UCSF Fresno, and within months his symptoms accelerated and the diagnosis was confirmed. "He would feel overwhelming fatigue, just walking across the room or taking a shower," a stark contrast from his regular lifestyle with long hours at work and frequent get-togethers with friends, said Allison, a business office manager at a law firm.
When Patrick's short-term survival became dire, Bilello arranged for his transfer to UCSF, where his treatment was overseen by Steve Hays, MD, medical director of the Lung Transplant Program. "Idiopathic pulmonary fibrosis is a relentless, progressive disease in which fibrous scar tissue builds up in the lungs, affecting the ability to provide oxygen. Without a transplant, patients may survive for around three to four years," he said. "But transplanted patients at UCSF, like Patrick, can live a normal life, with medications to ward off infections, healthy diet and exercise. I would expect Patrick to return to his previous lifestyle in about a year."
One week after surgery, Patrick was nipping around the hospital floor, minus the walker and minus the portable oxygen tank that had been his constant companion in the weeks prior to transplant. He's making plans again. He will return to work but will resume a lighter workload ("nobody is indispensable," he remarks with the wisdom of one whose future had hung in the balance not so long ago). And together with Allison, he will resume travel plans.
Back on the calendar: Ireland. The couple hopes that their third getaway attempt will be the charm.






