Blood sampling is a quick and accurate tool used to diagnose health conditions, like heart disease, diabetes, and liver function. Researchers at the UNC School of Medicine and Marsico Lung Institute/Cystic Fibrosis and Pulmonary Research Center have developed a tool that similarly monitors chronic lung conditions.
A new study published in NEJM Evidence, led by Mehmet Kesimer, PhD, a professor of pathology and lab medicine at the UNC School of Medicine, describes a new metric called the Quantitative Mucin Index (MUCQ) of the Lung. This tool analyzes sputum and other lung mucus samples to detect airway mucus abnormalities, assess disease risk, and track disease progression in patients over time.
"MUCQ allows us to detect underlying mucus abnormalities before significant lung damage appears on standard lung function tests," said Kesimer. "With an objective, biology-based measurement, we can now issue far more compelling evidence that will help physicians provide diagnoses and treatments sooner, rather than later."
The Role of Mucin in Lung Health

Mehmet Kesimer, PhD
Mucins are large proteins that make mucus slimy and thick. They play a crucial role, as the stickiness is what protects the respiratory system from pathogens, toxins, and physical damage. While mucins serve a protective function, excess and/or increased concentrations of mucins can restrict and block the airways.
This risk is heightened in individuals exposed to cigarette smoke and environmental allergens, which can trigger mucin/mucus overproduction and lead to chronic bronchitis, chronic obstructive pulmonary disease (COPD), or asthma. If left untreated, mucin hyperconcentration-related lung conditions can lead to serious health problems, so early detection is key before progressive, widespread airway obstruction develops.
However, the diagnosis of chronic bronchitis, a common precursor for COPD, currently relies on patient questionnaires that subjectively assess cough and phlegm history. Until now, physicians and researchers had no real, objective way to gauge a patient's risk of developing these kinds of lung diseases.
Quantitative Mucin Index of the Lung
Kesimer and co-authors from the nationwide COPD study, SPIROMICS, in the United States suggested that measuring two key airway mucins-MUC5AC and MUC5B-along with total mucin levels, may help identify risks associated with disease and determine disease progression.
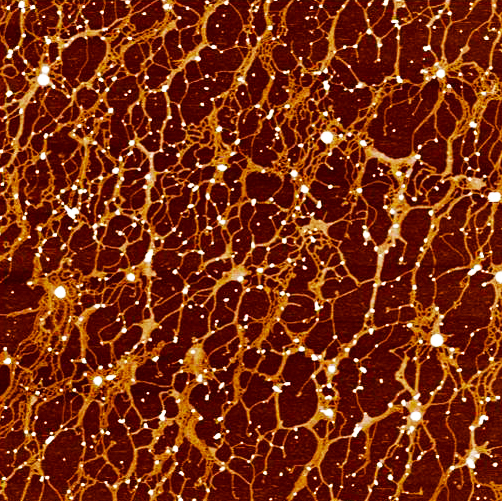
This mucus web, secreted by human lung tissue for protection, consists of large spaghetti-like mucin threads and thousands of other proteins. Measuring mucins has diagnostic and prognostic value. (Courtesy of Jerome Carpenter/Mehmet Kesimer)
Researchers then put their new score to the test. Using patient-derived samples from SPIROMICS they found that higher MUCQ scores sensitively and reliably indicated lung abnormalities and were linked to worse lung function, small airway disease, chronic bronchitis symptoms, and greater risk of future COPD exacerbations.
Importantly, elevated MUCQ values were also observed in symptomatic smokers with normal lung function, which suggests that MUCQ could be an accurate way to detect airway disease earlier than standard lung function tests.
Kesimer adds that the use of MUCQ score in clinical care may enable doctors to detect and track people who are at risk, giving them a chance to change their habits and lower their exposure before the disease develops or worsens.
"In the clinic, doctors always tell patients to stop smoking, but behavior change is hard," said Kesimer. "Being able to show a patient an objective numeric value -like their MUCQ score- especially when their lung function still appears normal, can be far more convincing."
"With MUCQ, we can identify and monitor at-risk populations, pushing them towards behavioral adaptations that would allow them to enjoy a higher quality of life and reduce the economic burden on the healthcare system."






