Personalized medicine is becoming the promise for better patient outcomes, and RNA-based drugs are leading the way, as they hold the potential to change the standard of care for many diseases.
RNA helps to turn genes on and off, aids in chemical reactions, slices and dices other RNA and even builds proteins, so harnessing this power for targeted therapy could open the door to new, powerful treatments. RNA vaccines are among those now being used to combat COVID-19.
But so far, these drugs haven't been quite as useful in getting through to the brain to treat tumors and other illnesses.
Researchers at the University of Cincinnati, in collaboration with the Georgia Institute of Technology and Emory University, have found that using ultrasound combined with RNA-loaded nanoparticles could help infiltrate the blood-brain barrier and deliver targeted, more effective treatment to brain tumors, while eliminating uncomfortable side effects.
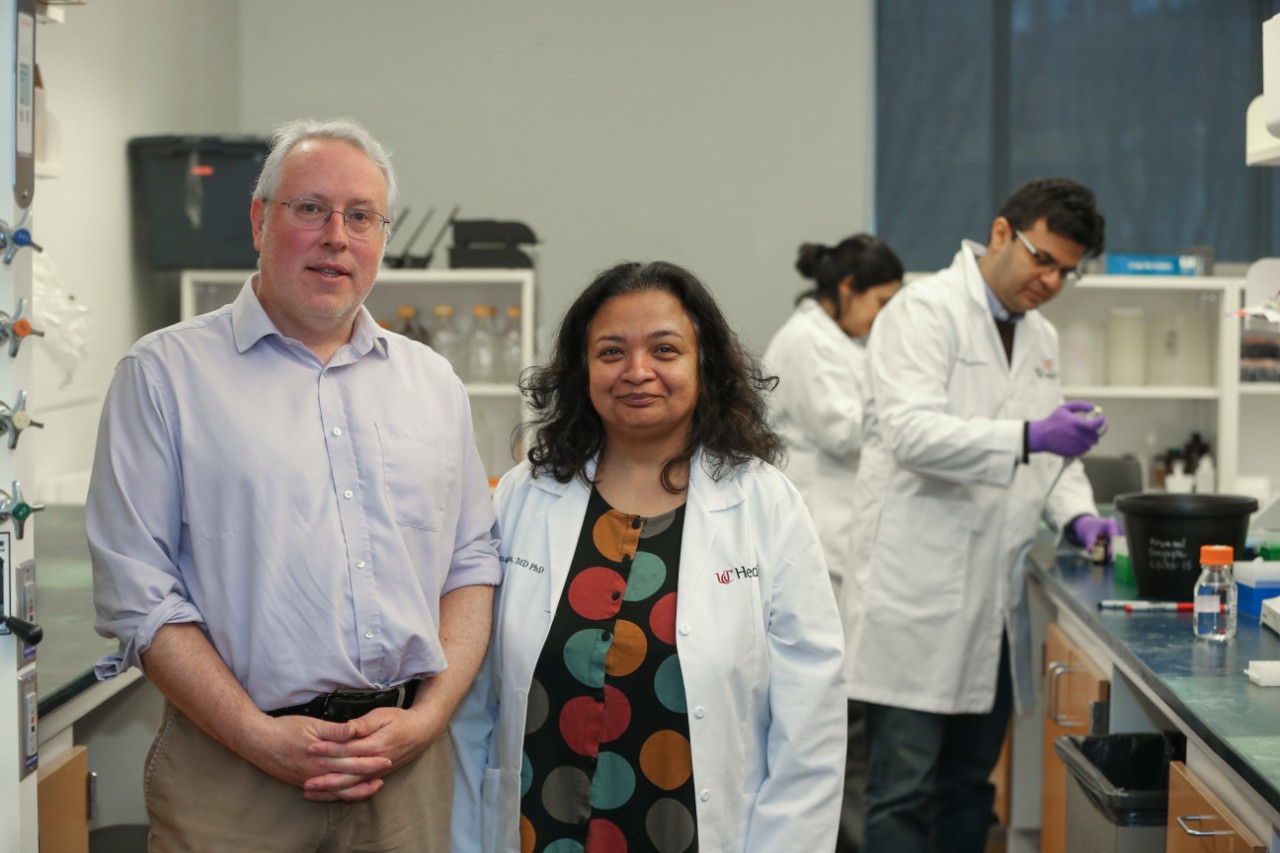
Daniel Pomeranz Krummel, PhD, research associate professor at UC, and Soma Sengupta, MD, PhD, associate director of the UC Gardner Neuroscience Institute's Brain Tumor Center, were integral contributors to this research, which could lead to better treatments for brain tumors. Photo credit/Joe Fuqua/UC Creative + Brand
The study was published in the journal Science Advances and could lead to new treatments for patients with a cancer that historically has poor outcomes: medulloblastoma, the most common brain tumor in children.
Soma Sengupta, MD, PhD, associate director of the UC Gardner Neuroscience Institute's Brain Tumor Center, and Daniel Pomeranz Krummel, PhD, were integral contributors to the research.
Pomeranz Krummel, research associate professor of neurology at UC, designed the RNA therapeutic used in the study. This is the first time that RNA therapeutics have been shown to successfully treat brain tumors.
RNA drugs have two major weaknesses: limited circulation time in the body and minimal absorption by cells. To overcome these challenges, researchers package the RNA drugs in nanocarriers, typically 100 nanometers in size, to improve their ability to be taken in by cells and delivered effectively. Still, these nanocarriers have been too large to penetrate the blood-brain barrier, the tightly connected and selective cells surrounding blood vessels in the brain, until now.
"RNA has enormous potential to function as a therapeutic to treat brain tumors," says Pomeranz Krummel. "But the challenge is getting the RNA to the tumor in adequate amounts and keeping it safe from degradation. We have potentially overcome both challenges."
Using animal models, the team used a modified version of ultrasound, the diagnostic imaging technique that uses sound waves to create images of internal body structures, such as tendons, blood vessels, organs and babies in utero.
Sengupta, associate professor of neurology at UC and UC Health neuro-oncologist, says this treatment could be especially desirable because it can be modified to fit the patient's needs - physicians can fine-tune the ultrasound pressure to control drug delivery. Also, it's noninvasive and very targeted in nature, because it's being delivered directly to the tumor.
"Being able to deliver this type of targeted treatment, without medicines running their course through a person's body, will help in eliminating potentially devastating side effects," says Sengupta, who is also the Harold C. Schott Endowed Chair of Molecular Therapeutics. "This technology has enormous potential in treating all kinds of brain cancers in adults and children. This can greatly change the way brain cancers are treated."
Following this study, Sengupta and Pomeranz Krummel are designing experiments with Haworth and co-authors at Georgia Tech and Emory to examine how this method can be used for treatment of tumors that are not able to be removed via surgery.
Featured photo: Image of microscopic nanoparticles loaded with RNA (left), illustration of RNA (middle), to target brain tumors (red-orange in the brain of illustration, right; credit: Ikumi Kayama). Provided by Pomeranz Krummel.
This work was supported by the National Institutes of Health (NIH), grant No. R00 EB016971 and grant No. R37 CA239039; and the CURE Foundation. Authors cite no conflicts of interest.






