When an invasive and deadly form of breast cancer called triple-negative grows, the fat cells around it seem to shrink.
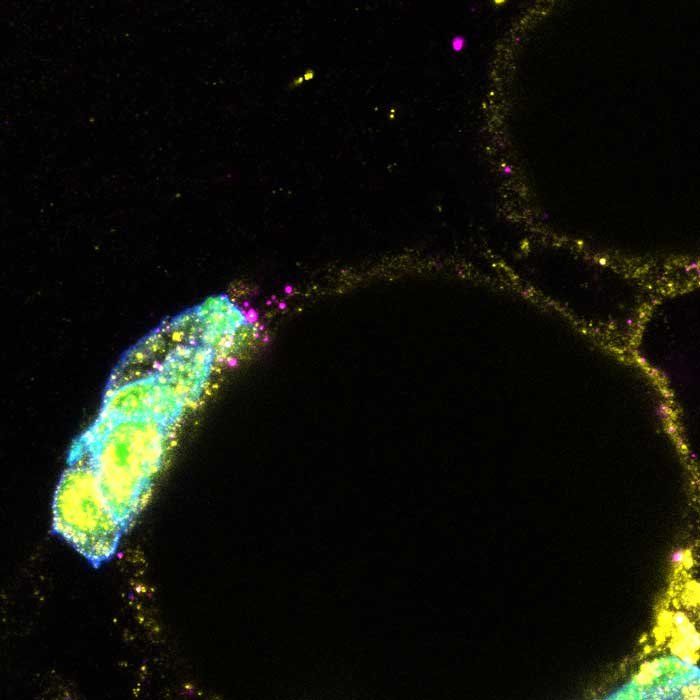
UCSF researchers have discovered that the cells of these tumors - so called because they test negative for estrogen, progesterone, and HER2 receptors - build molecular tunnels into nearby fat cells. The tumor cells then send instructions through the tunnels, which scientists call gap junctions, that trigger the fat cells to release stores of energy that could feed the cancer.
Blocking the gap junctions stopped tumors from growing, in the lab.
"Cancers thrive by hijacking the body's energy sources and we've identified how this works in triple-negative breast cancer," said Andrei Goga , PhD, professor of cell and tissue biology at UCSF, co-leader of the Breast Oncology Program in the UCSF Helen Diller Family Comprehensive Cancer Center, and senior author of the paper.
The study, which appears in Nature Communications on Aug. 20, was funded by the Department of Defense and the National Institutes of Health (NIH).
Goga and his team made their discovery by analyzing fat and tumor cells from breast cancer patients, as well as laboratory models of breast cancer.
The findings have immediate clinical implications. Although no one is yet testing drugs that block gap junctions for breast cancer, there are ongoing clinical trials using these drugs for brain cancer.
"This is a golden opportunity for us to develop effective strategies to treat the most aggressive forms of breast cancer."
Authors: Other UCSF authors are Jeremy Williams, Roman Camarda, PhD, Serghei Malkov, MSc,
Lisa J. Zimmerman, PhD, Andrew Beardsley, PhD, Daniel Van de Mark, PhD, Rachel Nakagawa, Yong Chen, MD, PhD, Celine Mahieu, PhD, Daphne Superville, Juliane Winkler, PhD, Elizabeth Willey, Erica J. Hutchins, PhD, John D. Gagnon, PhD, Seda Kilinc Avsaroglu, PhD, Kosaku Shinoda, PhD, Matthew Gruner, PhD, K. Mark Ansel, PhD, Zena Werb, PhD, Shingo Kajimura, PhD, Atul J. Butte, MD, PhD, Hope Rugo, MD, Gregor Krings, MD, PhD. For all authors see the paper.
Funding: This work was supported in part by the US Department of Defense (W81XWH-12-1-0272, W81XWH-21-1-0774), the National Institutes of Health (R01CA17447, 2R01EB028148, R01 CA056721, DK110426, R01CA166945, R01CA257652, F99CA212488, F31CA243468) the Atwater Foundation and Bechtle Family Foundation, the Breast Cancer Research Fund and Subramanian Breast Cancer Support Fund, and the European Molecular Biology Organization (ALTF 159-2017).






