Using human-induced pluripotent stem cell-derived kidney organoids, researchers from Science Tokyo uncovered how abnormal Hippo signaling drives fibrosis in nephronophthisis, a genetic kidney disorder caused by NPHP1 deficiency. Confirming their discovery, the team demonstrated that inhibiting the Hippo signaling pathway effectively suppresses fibrosis in kidney tissue. The study highlights the potential of organoid-based disease models for elucidating disease mechanisms while offering a new therapeutic target for nephronophthisis.
Hippo signaling pathway: A therapeutic target for NPHP1-deficient nephronophthisis (NPH)
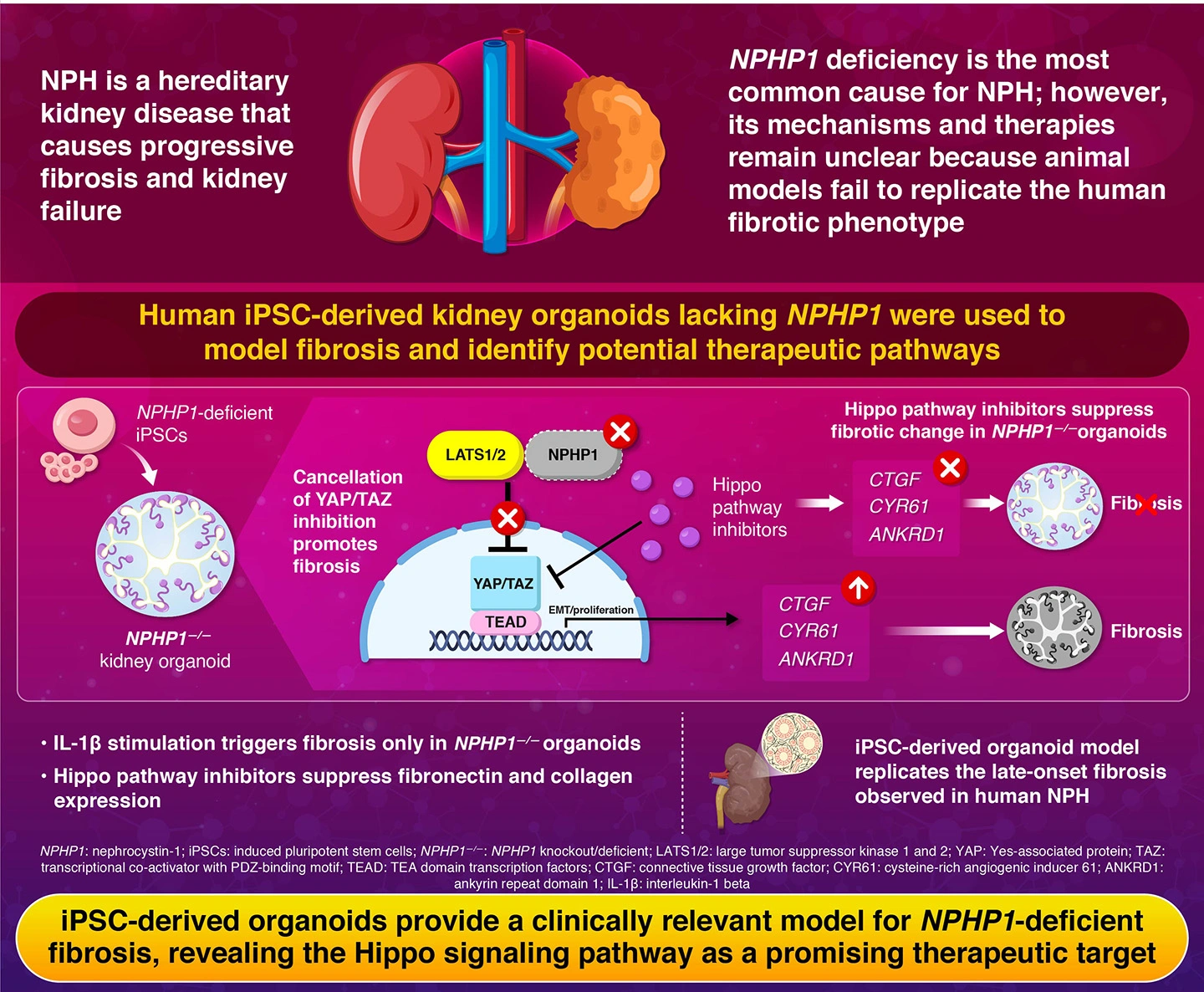
Nephronophthisis (NPHP) is a hereditary kidney disease characterized by progressive fibrosis of the kidney, which involves the abnormal accumulation of scar tissues within the kidney. It is one of the major causes of end-stage kidney disease in children and young adults, accounting for approximately 10% of all pediatric dialysis cases. Despite decades of research, there is no effective treatment available for NPHP to date, except for kidney transplantation.
The disease commonly arises from mutations or deletions in the NPHP1 gene, which provides instructions for making the nephrocystin-1 protein, essential for maintaining healthy kidney tubules. However, the exact mechanism underlying the disease has remained unclear because suitable animal models of NPHP1-related NPHP fail to reproduce the severe fibrotic changes seen in human patients.
To overcome this long-standing challenge, a research team led by Associate Professor Eisei Sohara, along with Junior Associate Professor Koichiro Susa and graduate student Takefumi Suzuki from the Department of Nephrology, Graduate School of Medical and Dental Sciences, Institute of Science Tokyo (Science Tokyo), developed a human-based kidney organoid model using human induced pluripotent stem (iPS) cells. Their findings were published in Volume 16, Article number 489 of the journal Stem Cell Research & Therapy on September 19, 2025.
"To model the NPHP1 deficiency observed in nephronophthisis, we used genome editing to remove the NPHP1 gene" explains lead author Sohara. "In this way, we generated NPHP1-deficient iPS cell lines which then differentiated into three-dimensional kidney organoids." These mini, self-organizing kidney structures could accurately mimic the architecture and cell composition of the human nephron.
When these NPHP1-deficient kidney organoids were exposed to low levels of inflammatory signals (interleukin-1β), they exhibited striking fibrotic changes that were not observed in normal kidney organoids. Detailed microscopic and molecular analyses revealed overexpression of fibrosis-related genes such as fibronectin, collagen, and CTGF, indicating activation of a key fibrosis signaling pathway in the NPHP1-deficient organoids.
Further investigation revealed abnormal activation of the Hippo signaling pathway in the NPHP1-deficient organoids. The Hippo signaling pathway is a molecular network that regulates tissue growth and repair, helping to prevent excessive scarring by controlling the activity of the YAP and TAZ proteins-the central activators of this pathway. The absence of NPHP1 disrupts this regulation, leading to uncontrolled fibrotic signaling.
"Our findings reveal that NPHP1 interacts with components of the Hippo pathway to maintain a balance between repair and fibrosis," says Sohara. "When this interaction is lost, the Hippo pathway becomes overactive, driving progressive kidney damage."
To explore the therapeutic potential of blocking this pathway, the team tested several Hippo pathway inhibitors on the organoid model. Among them, verteporfin-a light-activated drug already approved for treating a common eye condition called macular degeneration-was also tested. Strikingly, verteporfin effectively reversed fibrosis markers and also reduced accumulation of fibrosis-related genes. "Since verteporfin is already in clinical use, it offers an immediate treatment option for nephronophthisis," notes Susa.
Overall, the research marks a major step toward translating stem cell research into practical therapies for rare kidney diseases. As the first study to successfully test drugs on a human iPSC-derived NPHP model, it demonstrates how organoid technologies can replace animal models for more precise disease modeling and personalized drug testing.
In the future, the researchers plan to improve their kidney organoid platform to study additional signaling pathways and test more drug candidates for kidney fibrosis, paving the way for safer and more effective treatments for chronic kidney diseases.
Reference
- Authors:
- Takefumi Suzuki 1, Koichiro Susa1*, Hiroaki Kikuchi1, Yuta Nakano1, Tomoki Yanagi1, Yu Hara1, Tamami Fujiki1, Fumiaki Ando1, Shintaro Mandai1, Yutaro Mori1, Takayasu Mori1, Hiroaki Iwasa2, Yutaka Hata3, Shinichi Uchida1, Eisei Sohara1*
- Title:
- iPSC-based drug discovery identified the Hippo signaling pathway as a therapeutic target in the fibrosis of NPHP1-deficient nephronophthisis
- Journal:
- Stem Cell Research & Therapy
- Affiliations:
- 1Department of Nephrology, Graduate School of Medical and Dental Sciences, Institute of Science Tokyo, Tokyo, Japan
2Research and Development Division, Perseus Proteomics Inc, Tokyo, Japan
3Preventive Medical Center, Sunkohkai Medical Corp. Koga Community Hospital, Yaizu, Shizuoka, Japan






