A molecule made by bacteria in the gut can hitch a ride to the kidneys, where it sets off a chain reaction of inflammation, scarring and fibrosis - a serious complication of diabetes and a leading cause of kidney failure - according to a new study from researchers at the University of Illinois Urbana-Champaign and Mie University in Japan.
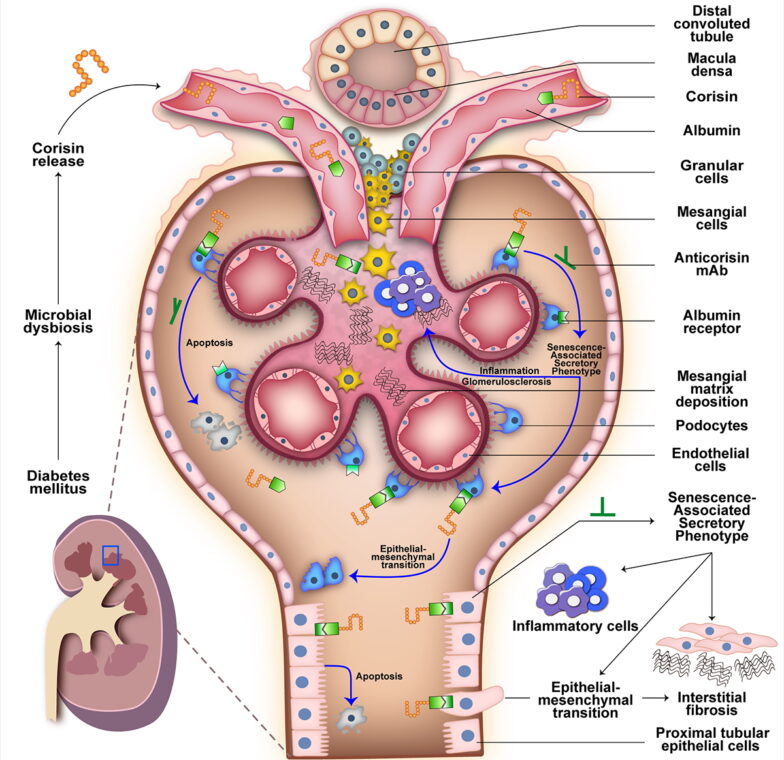
After finding high levels of corisin - a small peptide produced by Staphylococcus bacteria in the gut - in the blood of patients with diabetic kidney fibrosis, the researchers used computer simulations and tissue and mouse experiments to track how corisin affects the kidneys, how it gets there from the gut, and a possible method of countering it with antibody treatment.
"Our earlier studies showed corisin can damage cells and worsen tissue scarring and fibrosis in other organs, so we suspected it might be a hidden driver of kidney fibrosis," said Illinois animal sciences professor Isaac Cann, who led the study with Mie University immunology professor Dr. Esteban Gabazza. Cann and Gabazza are affiliates of the Carl R. Woese Institute for Genomic Biology at Illinois. "Our new findings suggest corisin is indeed a hidden culprit behind progressive kidney damage in diabetes, and that blocking it could offer a new way to protect kidney health in patients."
The researchers published their findings in the journal Nature Communications.

Diabetic kidney fibrosis is a major cause of kidney failure worldwide, yet the key drivers of it have remained a mystery, and no treatments can stop the process, said Dr. Taro Yasuma of Mie University, a medical doctor and the first author of the manuscript.
"Many people with longstanding diabetes eventually develop kidney fibrosis, and once it progresses, there are limited options beyond dialysis or kidney transplantation. Current treatments mainly focus on controlling blood sugar and blood pressure, but there's no cure that stops or reverses the scarring or fibrotic process," Yasuma said.
The researchers began by screening the blood and urine of patients with diabetic kidney disease. They found that patients had significantly more corisin than their healthy counterparts, and that the amount of corisin in the blood correlated with the extent of kidney damage.
Upon seeing the same results in mice with kidney fibrosis, the researchers tracked what corisin was doing in the kidneys of the mice. They found that corisin speeds up aging in kidney cells, setting off a chain reaction from inflammation to cell death to a buildup of scar tissue, eventually resulting in the loss of kidney function and worsening fibrosis.
But how was corisin getting from the gut to the kidneys? Cann and Gabazza's groups collaborated with U. of I. chemical and biomolecular engineering professor Diwakar Shukla's group to produce computer simulations and laboratory experiments to follow corisin's journey from the gut to the bloodstream. They found that corisin can attach to albumin, one of the most common proteins in blood, and ride it through the bloodstream. When it reaches the kidneys, corisin detaches from the albumin to attack the delicate structures that filter blood and urine.
To confirm that corisin was the main culprit behind the kidney damage, the researchers gave the mice antibodies against corisin. They saw a dramatic reduction in the speed of kidney damage.
"When we treated the mice with an antibody that neutralizes corisin, it slowed the aging of kidney cells and greatly reduced kidney scarring," said Gabazza, who also is an adjunct professor of animal sciences at Illinois. "While no such antibody is currently approved for use in humans, our findings suggest it could be developed into a new treatment."
Next, the researchers plan to test anticorisin treatments in more advanced animal models, such as pigs, to explore how they could be adapted for safe use in humans. The U. of I. and Mie University have a joint invention disclosure on corisin antibodies.
"Our work suggests that blocking corisin, either with antibodies or other targeted therapies, could slow down or prevent kidney scarring in diabetes and thus enhance the quality of life for patients," Cann said.
This study was supported by the Japan Science and Technology Agency, the Japan Society for the Promotion of Science, the Takeda Science Foundation, the
Japan Association for Diabetes Education and Care, the Eli Lilly Japan Innovation Research Grant, the Daiwa Security Foundation and the Charles and Margaret Levin Family Foundation. Cann is also a professor of microbiology and nutritional sciences and a member of the Center for East Asian and Pacific Studies at Illinois.






