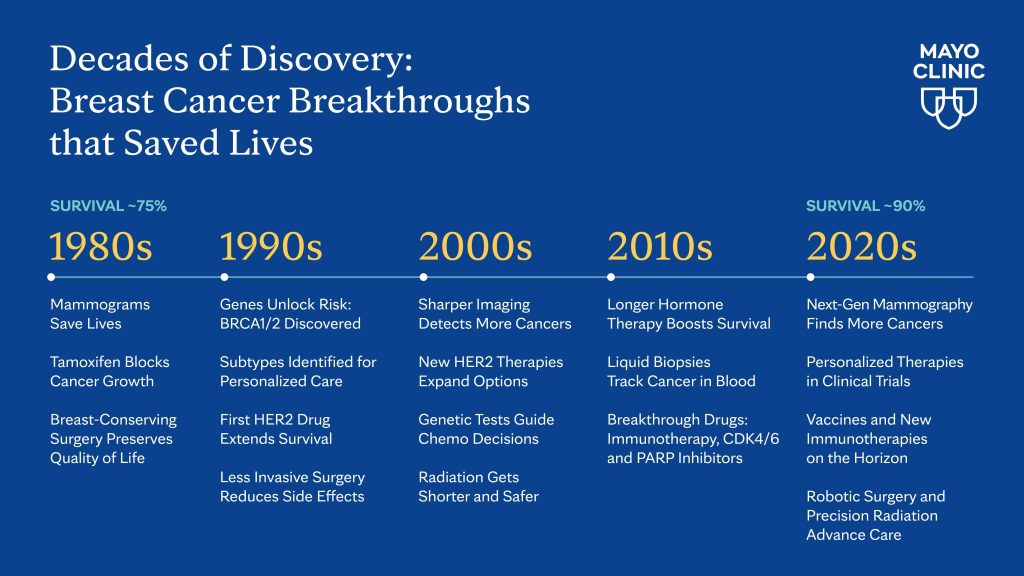
For more than 40 years, Mayo Clinic has been at the forefront of breast cancer innovation, transforming a once-limited diagnosis into a story of record survival rates, groundbreaking therapies and renewing hope for millions of patients worldwide.
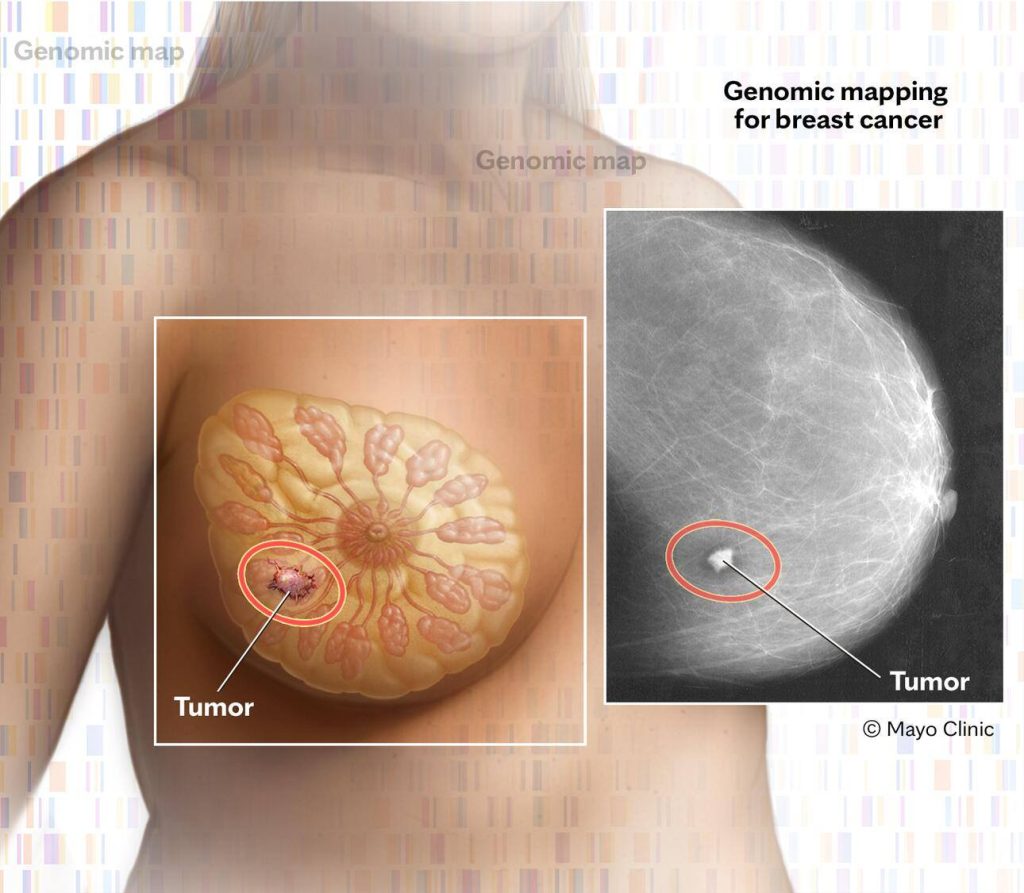
Detecting cancer earlier
Mammography revolutionized breast cancer care in the 1980s by finding tumors earlier, making them more treatable. Advances in digital mammography and 3D tomosynthesis have since improved accuracy, reduced false alarms and revealed cancers hidden in dense breast tissue.
Genetic testing has also reshaped care. Discoveries of BRCA1 and BRCA2 mutations - and later, additional genetic markers - have allowed healthcare teams to personalize screening and prevention. Mayo Clinic Comprehensive Cancer Center researchers, such as Siddhartha Yadav, M.B.B.S., M.D., and Fergus Couch, Ph.D., have helped refine risk predictions so patients and care teams can make more informed choices about surgery, surveillance or medication.
"By offering more precise, individualized risk estimates, our work supports shared decision-making between patients and their care teams to reduce the risk of breast cancer," says Dr. Yadav, a Mayo Clinic medical oncologist. He is expanding this work to better understand how inherited genetic changes influence tumor biology, treatment response and long-term outcomes in breast and ovarian cancers.
New tools such as contrast-enhanced digital mammography, which uses a special dye along with mammography, are showing promise in detecting cancers that traditional scans may miss. Bhavika Patel, M.D., a Mayo Clinic radiologist, is leading clinical trials that show its potential to move toward more personalized screening. "We aim to match the right test to the right woman at the right time because earlier detection means treatment can start sooner, which improves outcomes and saves lives," says Dr. Patel.
Dr. Yadav and Dr. Patel predict that over the next 10 years, risk assessment and breast imaging will work together to become even more personalized and integrated with artificial intelligence (AI) to tailor care and improve outcomes for every patient.
Understanding breast cancer subtypes
In the 1990s, researchers discovered that breast cancer is a collection of biologically distinct subtypes: hormone receptor-positive, HER2-positive and triple-negative breast cancer (TNBC). This opened the door to more personalized treatment.
At Mayo Clinic, researchers are now pushing this even further with studies led by breast medical oncologists Roberto Leon-Ferre, M.D., and Matthew Goetz, M.D., that suggest people who have early-stage TNBC and high levels of immune cells within their tumors (called immune infiltrating cells or TILs) may have a lower risk of recurrence and better survival rates even when not treated with chemotherapy.
Based on this work, Mayo Clinic Laboratory of Medicine and Pathology routinely reports TILs in all patients with early-stage TNBC. And Dr. Leon-Ferre and Dr. Goetz are developing a national clinical trial to evaluate TIL levels in patients with stage 1 TNBC. "The data will inform whether patients need or do not need chemotherapy, and could change standard practice," says Dr. Leon-Ferre.
New treatments, better outcomes
Tamoxifen was one of the first breakthroughs in hormone-targeted therapy. Two decades later, trastuzumab transformed outcomes for HER2-positive breast cancer. And new classes of drugs - including hormone therapies like aromatase inhibitors, CDK4/6 inhibitors, PARP inhibitors and immunotherapies - have dramatically extended survival for many patients.
Mayo Clinic researchers are leading national trials of next-generation therapies, like Dr. Goetz's study of drugs that more effectively block or degrade the estrogen receptor. Other trials are testing whether lower doses of tamoxifen can reduce side effects while still decreasing risk of further breast cancer events.
Tufia Haddad, M.D., breast medical oncologist at Mayo Clinic Comprehensive Cancer Center, is leading efforts to identify novel therapies to transform cancer care, such as showing the Aurora A kinase inhibitor, alisertib, can reduce or eradicate breast cancer stem cells within a tumor to shrink or stabilize the disease. She is now studying it in combination with different endocrine therapies, in hopes that a lower dose with fewer side effects will be better for patients.
Further, Saranya Chumsri, M.D., also a breast medical oncologist at the cancer center, is leading vaccine clinical trials in HER2-positive and TNBC that may one day prevent cancer from returning altogether.
"In 10 years, we will see growth of a new class of targeted treatment approaches to intercept cancer that is detected at a microscopic stage. Preventing cancer will become the new cure," says Dr. Haddad.
Smarter chemotherapy and genomic testing
Chemotherapy has become smarter and more tolerable with advances like shorter intervals between chemotherapy cycles and better supportive care. Mayo Clinic researchers are now exploring optimized treatment schedules and new combinations.
Genomic tests such as Oncotype DX analyze tumor biology to predict whether chemotherapy will help, sparing many women from unnecessary treatment. Liquid biopsies - blood tests that detect cancer DNA - are beginning to guide real-time treatment decisions.
Advances in surgery and radiation
Surgery and radiation also have evolved with a focus on survival and quality of life. Research proved that breast-conserving surgery with radiation was as effective as mastectomy, and sentinel lymph node surgery reduced the need for extensive operations, sparing many patients from long-term complications.
Judy Boughey, M.D., surgical oncologist and chair of Breast and Melanoma Surgical Oncology at Mayo Clinic Comprehensive Cancer Center, led a national study in the 2010s that dramatically changed the management of breast cancer for advanced disease, allowing even more patients to avoid axillary lymph node dissection.

Newer surgical techniques - skin- and nipple-sparing mastectomy, immediate reconstruction, and robotic approaches - are designed with both survival and quality of life in mind. James Jakub, M.D., surgical oncologist, performed the first robotic nipple-sparing mastectomy at Mayo Clinic in 2021 as part of a national clinical trial. Now, Mayo Clinic is the highest enrolling site in this clinical trial with principal investigator Mara Piltin, D.O., a Mayo Clinic surgical oncologist.
"These are significant advances, and in the future, we hope to eliminate surgery within the axilla (armpit area), use ablative therapies for tumors, inject medicines directly into the tumor and preserve sensation to the nipple-areolar during mastectomy," says Sarah McLaughlin, M.D., breast surgical oncologist at Mayo Clinic Comprehensive Cancer Center.
Radiation also has become more precise and efficient, with shorter treatment courses and advanced options such as proton therapy. Mayo's Proton Beam Therapy Program has treated 10,000 patients in 10 years - far exceeding national averages - and new technologies like carbon ion therapy are on the horizon.
A future of hope
Since 1989, breast cancer deaths in the U.S. have dropped nearly 40%. That progress is the result of decades of discovery - better imaging, smarter drugs, less invasive surgery and personalized medicine.
"Breast cancer care is one of the fastest-evolving areas in medicine," says Dr. Boughey. "Every clinical trial takes another step forward to improve outcomes and reduce side effects for patients."
For patients with breast cancer and their families, the last four decades tell a story of hope: survival is higher than ever, treatment is more personalized, and the future has never looked brighter.






