
For decades, it was impossible for clinicians to know which babies with major heart defects might eventually have developmental abnormalities, like ADHD and learning differences. Now, by adapting a simple and safe oxygen test, UC San Francisco researchers believe they can identify those most at risk, potentially leading to early detection and life-changing treatments.
Heart defects, also known as congenital heart disease (CHD), are the most common type of birth defect in the U.S., affecting nearly 40,000 births per year. Babies with CHD commonly experience abnormal brain development - such as brain injuries and smaller brain volumes - which are strongly correlated with developmental abnormalities.
A new study, led by researchers at UCSF Benioff Children's Hospitals and funded by the National Institutes of Health (NIH), examined the brains of babies with CHD. By giving extra oxygen to pregnant women and their babies before birth, researchers were able to measure the response in the fetal brain's blood vessels - a marker of brain health.
Brain MRI performed before birth and shortly after birth showed that babies with CHD who did not respond normally to the increased oxygen in the womb were more likely to have brain injuries than those who responded. The study, published in the Journal of the American Heart Association , also found that babies who did not respond to the increased oxygen and had a severe type of CHD had brain volumes that were significantly smaller than those who responded.
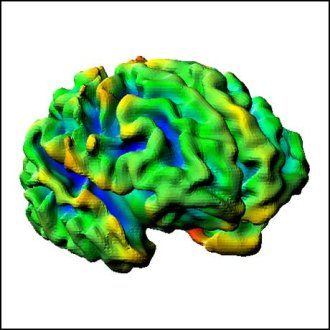
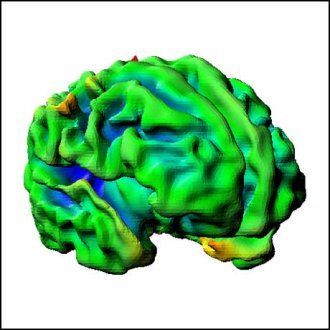
The figures below are of brain development at 40 weeks of gestation (at-term). The left shows "normal" fetal brain development without congenital heart disease, while the right shows less defined development with hypoplastic left heart syndrome (HLHS), a type of congenital heart disease.
"Although funding lags for pregnant women and their babies with heart defects, increased federal funding could turn research into early treatments that optimize brain development for children most at risk for developmental complications, and offer hope to families," said Shabnam Peyvandi , MD, MAS, a pediatric cardiologist at UCSF Benioff Children's Hospitals and senior author of the paper.
To treat babies with CHD and abnormal brain development, pediatric heart and brain specialists currently focus on the post-birth period. However, many babies with CHD have less developed brains before birth and incur brain injuries after birth. These early injuries are leading researchers at UCSF's Pediatric Heart and Brain Research Group to explore treatments before birth in hopes of preventing damage before it begins. While the extra oxygen test, known as maternal hyperoxia, can be used to help identify which children are most at risk, researchers still don't know which interventions might protect and grow fetal brains.
"Now that we can better identify children at risk, we need to prioritize nature and nurture to truly optimize brain health among children with heart defects by identifying neuroprotective interventions before birth, including resources for mothers," said Peyvandi.
One of these resources is UCSF Benioff Children's Hospital's Healthy Hearts and Minds (H2M) Program . H2M helps families and patients manage developmental challenges once they start by offering school resources, social work support, and nutrition counseling.
Authors: Please see the paper for a full list of authors.
Funding: National Institutes of Health (K23 NS099422 and R01 NS125404)
Disclosures: The authors declared no conflicts of interest.






