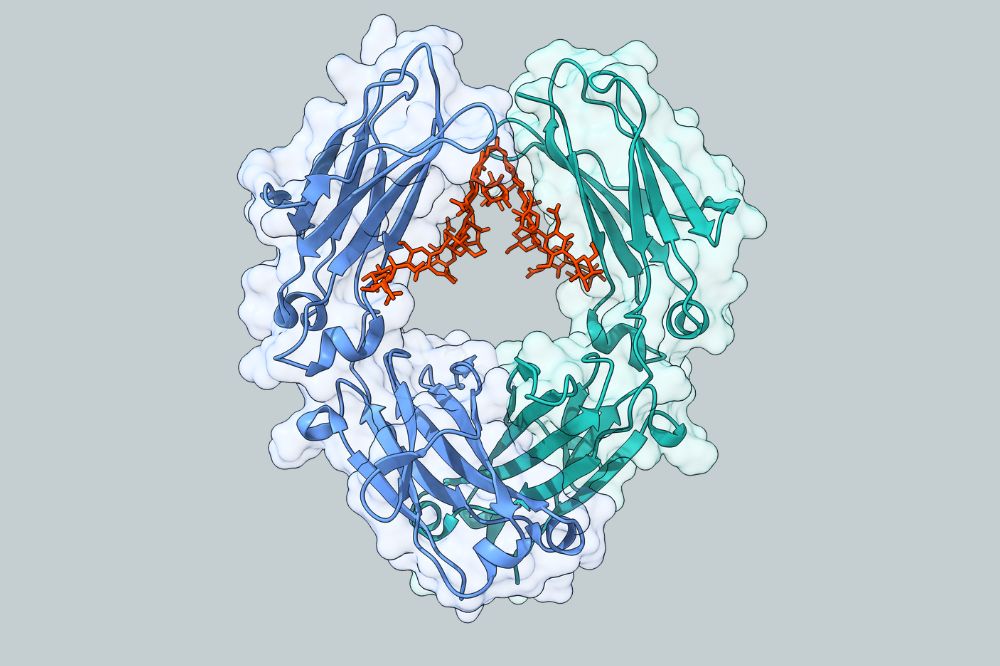
The Ravetch lab engineered an antibody therapy based on the insight that antibodies containing a specific sugar group, sialic acid, can foster an anti-inflammatory state through co-engagement of Type I and II Fc receptors. (Credit: Ravetch lab)
As many as 50 million Americans suffer from one or more autoimmune conditions, according to recent studies, a number that's increasing by up to 12 percent each year. Yet existing treatments are either difficult to administer or broadly suppress patients' immune systems-creating a huge unmet need for better therapies.
Nuvig Therapeutics, a biotech startup cofounded and advised by Rockefeller scientist Jeffrey Ravetch, aims to meet it.
Since launching in 2022, the California-based company has raised more than $200 million and launched two phase 2 trials to evaluate a new treatment for autoimmune disease that avoids the practical limitations and unwanted side effects of existing therapies.
Nuvig's lead drug candidate is based on research that Ravetch, head of the Leonard Wagner Laboratory of Molecular Genetics and Immunology, began publishing 25 years ago.
Ravetch is an expert on the Fc domain, a structural component of antibodies that plays a crucial role in activating immune responses. His work has been used to enhance numerous cancer drugs and to develop a novel cancer immunotherapy that is in clinical trials.
While investigating the mechanism behind intravenous gamma globulin (IVIG), a liquid antibody cocktail derived from human plasma that is used to treat autoimmune diseases like lupus and multiple sclerosis, Ravetch discovered that a small fraction of those antibodies possessed a naturally occurring modification to their Fc. By engineering the Fc in his lab, Ravetch was able to create a molecule that was ten times more potent than IVIG.
The potential therapeutic benefits were clear. IVIG is used to treat scores of autoimmune diseases that afflict millions of people worldwide. And it is the only autoimmune therapy that does not broadly suppress the immune system, leaving patients more vulnerable to infections and cancer.
But IVIG has serious drawbacks. Because it is made from donated human plasma, it is expensive and prone to shortages. And because so few antibodies contain the Fc modification that Ravetch identified, IVIG must be administered in massive quantities: Infusions can take up to 10 hours, chaining patients to their IV bottles for days at a time.
"You basically have to put your life on hold," Ravetch says.
Some patients can't cope with the sheer quantity of liquid protein involved, causing physicians to prescribe a less-than-optimal dose. And some conditions would require such high doses that IVIG simply isn't practical.
"There are a lot of autoimmune diseases where IVIG probably would work but can't be tolerated because patients can't take the protein load or fluid volume," says Nuvig cofounder and chief scientific officer Pamela Conley.
Because Ravetch's engineered Fc fragments could be synthesized in large quantities, they would sidestep IVIG's supply issues. And because they are so potent, they could be administered in much smaller quantities, unchaining patients from their IVs: Infusions in Nuvig's trials take one hour rather than five, and for some conditions a self-administered subcutaneous injection might suffice.
Conley, who formerly served as an executive at a company Ravetch was advising, recognized that this research could be used to develop a therapy that had all the benefits of IVIG and none of its shortcomings. So she and a colleague teamed up with Ravetch to form Nuvig.
The drug they developed, NVG-2089, is currently being evaluated as an IVIG substitute for two autoimmune diseases: a debilitating neurological condition called chronic inflammatory demyelinating polyneuropathy that accounts for more than $4 billion in annual sales for IVIG; and immune thrombocytopenia, a rare blood disorder that causes bruising and bleeding.
Conley says that NVG-2089 ought to work everywhere IVIG does, and its potency would allow it to be used against autoimmune diseases where IVIG is impractical. The company has a list of conditions it would like to pursue in the near future, including a pair of painful, blistering skin diseases that have few treatment options. And it is exploring the possibility of using Ravetch's research to enhance other antibody-based autoimmune drugs, including ones being developed for use against common conditions such as rheumatoid arthritis and irritable bowel disease.
In the meantime, Ravetch has continued to explore the natural anti-inflammatory pathway that IVIG exploits. In a recently published study, he describes a fresh insight into the molecular mechanisms at play that has allowed him to achieve an additional tenfold increase in potency over IVIG, raising the possibility of an even more robust and widely applicable compound down the road: If Ravetch can help Nuvig use this latest breakthrough to create a second-generation therapy that's 100 times more powerful than IVIG, the dosage could drop so low that a single injection every couple of weeks might suffice to treat an even broader array of autoimmune conditions-all without making patients sick in the process.
"Patients with autoimmune disease deserve something better," Conley says.






